Dr Arpan Ashok Patel – Financial Toxicity: Impact on Older Adults with Advanced Cancer
Dr Arpan Ashok Patel of the University of Rochester School of Medicine and Dentistry is dedicated to better understanding the prevalence and impact of financial toxicity amongst older, more advanced cancer patients. His recent work in this field is the first to analyse real conversations between patients and oncologists in this high-risk group. His findings show that those struggling with financial stability following cancer treatment are more likely to have a lower health-related quality of life, highlighting the need for better screening tools to identify at-risk patients to allow appropriate signposting to support.
Receiving a cancer diagnosis is a devastating blow. Although patients should be focusing on their treatment, their thoughts often turn to finances, especially if they are without insurance or are not eligible for government support. In 2011, the Centers for Disease Control and Prevention found that nearly one-third of families in the USA reported having financial burdens related to healthcare costs. Moreover, around 10% had medical bills that they were unable to pay.
Cancer is one of the most expensive diseases to treat. Treatment costs are much more likely to be patient-funded than for other chronic diseases. After receiving a diagnosis, out of pocket medical expenses can increase exponentially up to tens of thousands of dollars. Even those with Medicare, an American government health care plan for the elderly, are likely to experience high out of pocket expenses for cancer treatment, especially if they do not have any supplementary insurance. A recent study revealed that one in every ten cancer patients with Medicare pays expenses that equate to 60% of their household income. Patients with private insurance may also experience additional costs due to being underinsured or exceeding the cover threshold.
The intensive and lengthy nature of treatments such as chemotherapy may lead to cancer patients losing their employment. Without a regular income, patients may have to resort to withdrawing retirement funds, selling their homes or even filing for bankruptcy. Sometimes, patients question if they will be able to afford to continue treatment. This adds extreme emotional stress on top of the physical stresses endured throughout their treatment journey.

What is Financial Toxicity?
Financial toxicity refers to the monetary burden of paying for cancer care costs and the negative impact of this on patient financial stability. Although the impact of financial toxicity upon cancer survivors has not been widely researched, in 2014, a large-scale study reported that almost half of cancer patients taking part were having difficulties living on their household income. Furthermore, those with a high financial burden were likely to be experiencing a poorer quality of life.
Dr Arpan Patel from the University of Rochester School of Medicine and Dentistry, works in the field of oncology and believes we should not overlook the impact of the financial strain upon cancer patients. He has witnessed first-hand the relationships between patient distress, financial toxicities and quality of life when treating complex illness. Recently, Dr Patel has been involved in research focusing on the impact of financial toxicity upon older adults with advanced cancer.
Older and More Advanced Patients
Older adults are likely to face a different set of pressures than those of younger patients. Their main source of income is typically either from the government or from private retirement savings (which may be in the form of a pension). In the USA, all over 65s are entitled to Medicare. However, this government financial assistance does not cover all healthcare expenditures, meaning patients have to make up potential shortfalls out of their own pockets. Cancer is also more prevalent in this age group, and the rate of prevalence in older adults is growing. Indeed, the worldwide cancer diagnosis amongst over 65s is predicted to double by 2035.
Previous research has identified two key and important themes in relation to financial toxicity amongst older adults. This first is that patients who report financial toxicity are more likely to have a lower health-related quality of life. The second is that patients often wish to discuss treatment expenses with their oncologists but these conversations rarely take place due to healthcare providers’ discomfort.
Dr Patel and his colleagues wanted to focus their research on the experiences of older and more at-risk cancer patients. They aimed to assess the prevalence of financial toxicity in older advanced cancer patients and to examine the relationship between financial toxicity and health-related quality of life. In addition, they wanted to understand more about the financial conversations between these patients and their oncologists.

Ascertaining the Prevalence of Financial Toxicity
Dr Patel asked questions about financial hardship to ascertain whether patients met the criteria for financial toxicity. The main questions asked about treatment delays due to financial issues and levels of income for food and housing, as well as for clothing, medicine, repairs to the house and transport. The researchers found that almost 20% of patients over the age of 70 with advanced cancer had experienced financial toxicity. The data also suggested this was more likely to be experienced by those who were female, Black/African American, single, had a lower average household income, had a lower level of education, were not employed and whose health costs were covered by Medicare alone.
It is important that healthcare providers use screening tools to assess if patients are at risk of financial toxicity. Dr Patel and his colleagues believe that if validated, even the simple financial hardship questions used in this study could be an effective way of identifying the most at-risk patients.
Assessing Health-Related Quality of Life
As part of the study, patients also undertook various assessments to measure their health-related quality of life. These assessments examined how a persons’ physical, mental, emotional and social functioning affected their health, comfort and ability to participate in or enjoy life events. Dr Patel and his colleagues found that patients with financial toxicity were likely to report higher levels of mental health issues such as depression, anxiety and distress. In line with previous research, they found that in this high-risk group, those with financial toxicity were more likely to have a poorer health-related quality of life.

The Importance of Cost Conversations
A unique part of the study was that at least one clinic visit between the oncologist and the patient was audio recorded. These recordings revealed that only 50% of patients experiencing financial toxicity had a conversation about costs or finances. Previous research has suggested that around 80% of patients wish to have this kind of conversation, indicating a gap between what the patient desires and practices. Why might this disparity exist? Dr Patel notes that both parties may be reluctant to bring up the subject of cost. For patients, there is the potential embarrassment of acknowledging they cannot afford treatment while oncologists may not feel comfortable about discussing this topic.
When the researchers examined the content of these conversations, four main themes emerged. The first was the cost of care, which was mainly initiated by the patient or caregiver. The second was about the patients’ ability to continue to work or provide for their household in relation to these costs. The third was typically initiated by the oncologist and focused on the patient ability to afford care. The final theme was about costs that were not treatment related.
Shockingly, almost 12% of oncologists dismissed cost conversations when patients or caregivers raised them. However, in the majority of cases, oncologists did offer interventions or signpost to other resources that would be able to help the patient. Dr Patel and his colleagues are keen to emphasise that direct discussions around cost can help prevent financial toxicity. These discussions can allow oncologists to share knowledge about external resources that can provide support, such as social workers, financial advisors, support groups, charities and co-pay assistance.

Addressing Financial Toxicity at the Policy Level
The findings from Dr Patel and his colleagues shine an important light on the extent to which older and more advanced cancer patients are experiencing financial toxicity and the negative impact this can have. Importantly, they identify that there is a clear need for proper screening tools that can identify patients who are at high risk of financial toxicity. Furthermore, they note that there is currently no routine training for healthcare providers and no standardised approach between organisations. As a result, Dr Patel believes that policy change is needed to ensure interventions relating to financial toxicity occur at a national level. Critically, the lack of adequate assessment, particularly in older people with advanced cancer, means that they cannot receive appropriate referrals to support.
SHARE
DOWNLOAD E-BOOK
REFERENCE
https://doi.org/10.33548/SCIENTIA760
MEET THE RESEARCHER

Dr Arpan Ashok Patel
School of Medicine and Dentistry
University of Rochester
Rochester, NY
USA
Dr Arpan Ashok Patel is a clinician who specialises in haematology and oncology. Currently, he is Assistant Professor in Thoracic-Oncology in the Department of Hematology Oncology at the University of Rochester’s Wilmot Cancer Center, where he also serves as Chief Quality Officer for the Division of Hematology Oncology and Associate Director for Informatics for Department of Medicine. Dr Patel gained his MD at the Medical University of Lublin in Poland in 2012 and then completed training in internal medicine at SUNY Upstate Medical University in New York, staying on for an additional year as Chief Resident. Dr Patel then undertook his fellowship training in haematology oncology with the University of Florida in Gainesville, winning the Chief Fellow Award in 2019. His research interests include thoracic-oncology, quality improvement, financial toxicity, patient distress and education.
CONTACT
E: Arpan_Patel@URMC.Rochester.edu
W: https://www.urmc.rochester.edu/people/31621410-arpan-a-patel
KEY COLLABORATORS
Asad Arastu, MD, Department of Medicine, Oregon Health and Science University Hospital, Portland
Jeffrey L. Berenberg, MD, Hawaii National Cancer Institute Community Oncology Research Program, Honolulu
Joseph Ciminelli, MD, Department of Biostatistics, University of Rochester School of Medicine and Dentistry, Rochester, New York
Eva Culakova, PhD, Department of Surgery, Cancer Control, University of Rochester School of Medicine and Dentistry, Rochester, New York
David W. Dougherty, MD, MBA, Dana Farber Cancer Institute, Boston, Massachusetts
Paul Duberstein, PhD, Department of Health Behavior, Society, and Policy, Rutgers School of Public Health, Piscataway, New Jersey
Marie Anne Flannery, PhD, School of Nursing, University of Rochester School of Medicine and Dentistry, Rochester, New York
Valerie Aarne Grossman, BSN, RN, Division of Hematology/Oncology, James P Wilmot Cancer Institute, University of Rochester School of Medicine and Dentistry, Rochester, New York
Elaine Hill, PhD, Department of Public Health Sciences, University of Rochester School of Medicine and Dentistry, Rochester, New York
Charles Stewart Kamen, PhD, MPH, Division of Hematology/Oncology, James P Wilmot Cancer Institute, University of Rochester School of Medicine and Dentistry, Rochester, New York
Ramya Kaushik, BA, University of Rochester School of Medicine and Dentistry, Rochester, New York
Lianlian Lei, PhD, Department of Public Health Sciences, University of Rochester School of Medicine and Dentistry, Rochester, New York
Yang Liu, PhD, Department of Neurosurgery, University of Rochester, Rochester, New York
Kah Poh Loh, MBBCh, BAO, Division of Hematology/Oncology, James P Wilmot Cancer Institute, University of Rochester School of Medicine and Dentistry, Rochester, New York
Chintan Pandya, PhD, MPH, MBBS, Dana Farber Cancer Institute, Boston, Massachusetts
Mostafa R. Mohamed, MSc, Division of Hematology/Oncology, James P Wilmot Cancer Institute, University of Rochester School of Medicine and Dentistry, Rochester, New York; Department of Public Health Sciences, University of Rochester School of Medicine and Dentistry, Rochester, New York
Supriya Gupta Mohile, MD, Division of Hematology/Oncology, James P Wilmot Cancer Institute, University of Rochester School of Medicine and Dentistry, Rochester, New York
Megan Wells, BFA, Division of Hematology/Oncology, James P Wilmot Cancer Institute, University of Rochester School of Medicine and Dentistry, Rochester, New York
Huiwen Xu, PhD, Department of Surgery, Cancer Control, University of Rochester School of Medicine and Dentistry, Rochester, New York
ACKNOWLEDGEMENTS
The researchers extend their gratitude to the patients, oncologists and support staff who participated in this research. They also thank the University of Rochester National Cancer Institute Community Oncology Research Base network, members of SCOREboard, and the dedicated support of all members of the Geriatric Oncology research group at the University of Rochester. They would also like to thank the Cancer and Aging Research Group, especially Drs Tanya Wildes, Shabbir Alibhai, Tsang Mazie and Hira Mian, for their review of the published paper and feedback.
FUNDING
Patient-Centered Outcomes Research Institute
National Cancer Institute (National Institutes of Health)
National Institute of Aging (National Institutes of Health)
Wilmot Cancer Institute
FURTHER READING
A Asad, A Patel, S G Mohile, et al., Assessment of Financial Toxicity among Older Adults with Advanced Cancer, JAMA Network Open, 2020, 3(12), e2025810.

REPUBLISH OUR ARTICLES
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence (CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
SUBSCRIBE NOW
Follow Us
MORE ARTICLES YOU MAY LIKE
Dr Yong Teng | Improving the Outlook for Head and Neck Cancer Patients
Dr Yong Teng at the Emory University School of Medicine is working with colleagues to overcome the high mortality of individuals diagnosed with cancers affecting the head and neck. One of his approaches is based on understanding the particular mechanisms of the ATAD3A gene, which new insights suggest are closely related to cancers affecting the head and neck.
Professor Toni Miles | Why Understanding Bereavement Matters
Professor Toni Miles has dedicated her research efforts to measuring bereavement and its impact on population health. Individual experience with bereavement is commonplace, but we know little about its impact on society when there is an instantaneous experience by a large number of individuals, i.e., mass bereavement. To measure its occurrence, her research with colleagues first confirmed that bereavement can be effectively measured in population surveys. Professor Miles argues that we should use such approaches to deliver interventions aiming to reduce the negative consequences of bereavement on individuals. By measuring bereavement in communities, these data become a cost-effective way to increase resilience, reduce demands on healthcare systems, and enhance public safety.
Dr Omar Islam | Portable Magnetic Resonance Imaging: An Important Innovation
Imaging technologies are vital in modern medicine and have revolutionised how clinicians make diagnoses and monitor disease progression. However, the necessary equipment – such as a scanner for magnetic resonance imaging (MRI) – is very large and expensive, requiring patients to go to the scanner rather than receiving scans as bedside care. This takes up valuable staff time and resources, and can present further risks to patients. Dr Omar Islam from Queen’s University and Drs Aditya Bharatha and Amy Lin from the University of Toronto are showing how portable MRI scanners may offer a viable alternative that benefits patients and healthcare systems.
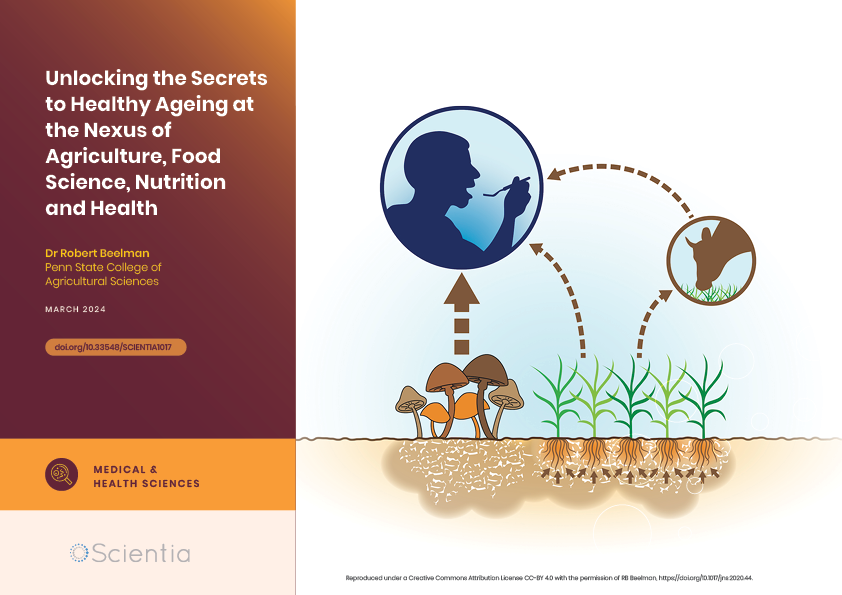
Dr Robert Beelman | Unlocking the Secrets to Healthy Ageing at the Nexus of Agriculture, Food Science, Nutrition and Health
Dr Robert Beelman is Professor Emeritus of Food Science and the Director of the Center for Plant and Mushroom Foods for Health at Penn State College of Agricultural Sciences. His groundbreaking research on the medicinal properties of mushrooms and vital nutrients like Ergothioneine has opened new pathways in understanding the link between diet, soil health, and human longevity.