Spirometry 360: Asthma Management Gets an Upgrade
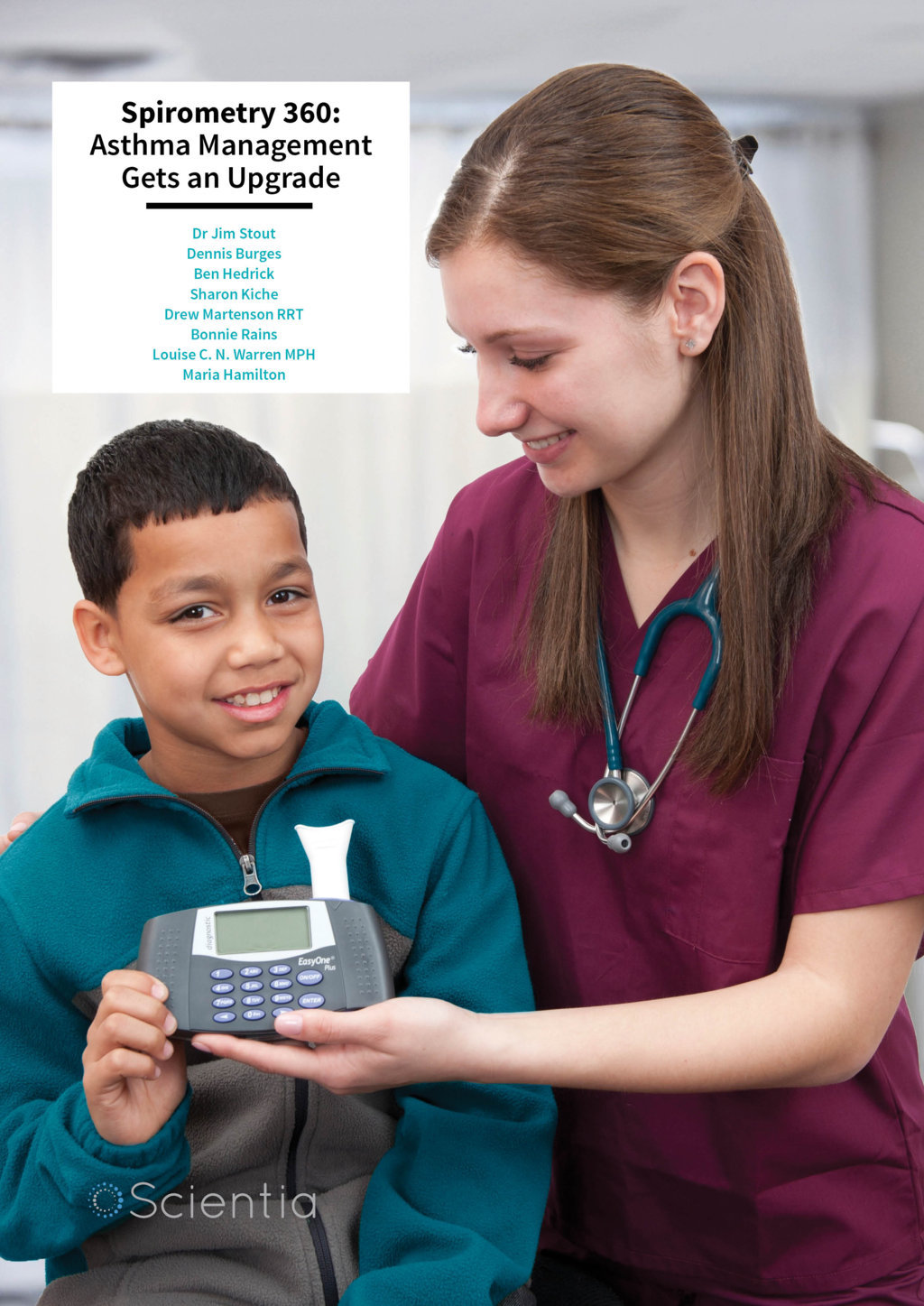
Dr Jim Stout and his multidisciplinary team at the University of Washington are on a mission to improve asthma care. Through novel training schemes, quality improvement methods and research into health disparities, these researchers are determined to reduce undertreatment and morbidity associated with asthma and lung obstruction.
Asthma affects approximately one in twelve individuals and most of us have someone in our lives who lives with the condition. Although common, it is important not to underestimate the impact that asthma can have on an individual’s life. So, what exactly is asthma? Asthma is a disease of the lungs in which the airways become irritated and inflamed causing them to tighten and contract. This leads to coughing, wheezing and breathlessness which vary in severity from person to person.
According to US guidelines, asthma can be categorised into four levels of severity: intermittent, mild persistent, moderate persistent and severe persistent. It is essential that individuals be correctly diagnosed, as choice of treatment will depend on the determination of severity. Underestimation leads to undertreatment, higher healthcare costs and increased morbidity and mortality. Severity is determined on the basis of symptom frequency and pulmonary function. In the past, pulmonary function was measured through peak expiratory flow (which measured how well your lungs could push out air) but the medical field has now moved away from peak flow meters as diagnostic devices. Compared to spirometry, peak flow provides far less accuracy and sensitivity in determining pulmonary function. Spirometry measures how much air your lungs push out and how quickly they do it. Studies have shown that spirometry is more reliable and has a higher correlation with the degree of airway obstruction than peak expiratory flow.

‘Our first trial of Spirometry Fundamentals taught us we needed a more comprehensive solution… from which we created Spirometry 360. We’ve trained about 300 practices domestically, and dozens of clinicians and support staff internationally.’
So how well do healthcare providers use these tools in the diagnosis and treatment of asthma in children? In a 2006 study, Dr Jim Stout and his colleagues aimed to find out. Their objective was to determine if adding these lung function measurements to clinical history substantially changed severity classification and treatment decisions. Although clinicians are recommended to use a combination of objective measurements and clinical findings, many rely more on the presentation of symptoms than the use of spirometry. The team measured what proportion of children in two cohorts were reclassified from less severe classifications to more severe classifications when lung function measurements were taken into account. They found that 22.8% and 27.7% of children in the mild intermittent category of each respective cohort would be reclassified to either moderate or severe persistent asthma when lung function was accounted for. Additionally, in both cohorts, approximately one third of children with mild persistent asthma would be similarly reclassified.
Several other studies have also reported that doctors systematically underestimate asthma severity, in part because they do not carry out spirometry tests with patients. ‘Although a recommended component of asthma care, spirometry is not routinely used in most primary care offices, and test quality and interpretation often leave room for improvement,’ Dr Stout states. Why is this happening? Many physicians cited a lack of time and training as the primary barriers. Faced with this problem, Dr Stout and his colleagues took action and began developing a quality improvement tool that would improve the overall diagnosis and management of asthma.
Developing Spirometry 360: An Online Training Program
Over time, Dr Stout gathered a multifaceted team to tackle the problem. Dr Karen Smith, Dennis Burges, Ben Hendrick, Sharon Kiche, Drew Martenson, Bonnie Rains and Louise Warren all contributed to the development of Dr Stout’s novel spirometry training program. Spirometry 360 offers a number of online courses and webinars that aim to improve the quality and frequency of spirometry testing in primary care practices. But given that it is delivered through an online platform, how well does such a program work?
In a study published in 2012, Dr Stout and his team (led by Dr Rita Mangione-Smith) evaluated the effectiveness of a virtually delivered quality improvement program for enhancing primary care management of children with asthma. They hoped that the program would lead to increased frequency and quality of testing, better documentation of asthma severity and improved prescription of controller medications. Participants received a CD-ROM on spirometry fundamentals, access to interactive webinars and feedback on spirometry quality. Feedback is the essential second prong of the program. The system allows the team to review and analyse spirometry tests from point of care and give appropriate technique feedback to the practitioner.
The results showed a significantly greater percentage of high quality tests in the group that participated in the program when compared to a control group. They were also 2.9 times more likely to document the severity of asthma, which had high concordance with appropriate treatment. This shows that successful quality improvement can occur through distance learning. ‘Since 2009, Spirometry 360 has been licensed to over 300 practices domestically and internationally,’ says Dr Stout. ‘Spirometry Fundamentals, our first training tool, is a compulsory part of a comprehensive spirometry training program in The Netherlands.’ With over 25,000 graded spirometry tests stored in the system, the team are now working towards developing a more sophisticated grading system based on machine learning techniques. The Spirometry 360 Feedback Reporting System has also been successfully integrated with SpiroSmart, a smartphone-based spirometer app in development, allowing for remote training and feedback.
Dr Stout is keen to acknowledge support for Spirometry 360 from the National Heart, Lung, and Blood Institute (NHLBI) over the years. ‘NHLBI has funded us three times – initially through two funded projects from the National Asthma Control Initiative (NACI), to initially deliver Spirometry 360 to “safety net” practices, and then to deliver a “train the trainer” Spirometry 360 program to four sites around the US,’ he explains. ‘NHLBI also funded an R-01 led by Dr Mangione-Smith, a controlled trial of the effect of Spirometry 360 on health outcomes among children and teens with asthma.’

Going International
Dr Stout is also a long-standing member of the International Primary Care Respiratory Group who are responsible for enabling numerous training relationships for Stout and his colleagues. In one such example, he and his team carried out a study between the University of Washington (where the researchers are based) and an outpatient clinic in Bangladesh. International collaborations such as these are made possible by grants from projects such as Horizon 2020 FRESH AIR, which aims to improve health outcomes associated with non-communicable lung diseases in low resource settings.
Spirometry is available in some low resource settings but there is limited training available on the use and interpretation of these measures. This is where Spirometry 360 comes in. Over the course of five months, the comprehensive online training and feedback program was used to improve the quality of spirometry in the Bangladeshi clinic. Facilitated by site leader Dr Monsur Habib, seven physicians and a medical assistant were trained with an online primer known as ‘Spirometry Fundamentals’, engaged in selfpaced learning labs and received feedback from the reporting system. Upon completion of their training, the results were significant. The useful test rate jumped from 85% to 91% and the ratio of grade A tests jumped from 66% to 77%.
Reducing Health Disparities Through Guideline Implementation
However, there is more to improving asthma management than just training physicians. In order to instigate true change, Dr Stout and his team at Seattle/King County Health Department are supporting practitioners and patients alike in implementing best practice guidelines for asthma management. This approach to asthma care is based on the results of several studies showing poor adherence to recommended guidelines and the influence of environmental and social factors, such as poverty, housing supply, race and geographical location, on asthma management.
Asthma can be controlled and guidelines for optimal care are available, but care often doesn’t live up to these standards. Poor adherence is a major problem amongst patients – only one third are compliant with their asthma controller medication, while only two thirds follow advice on reducing environmental asthma triggers. This particularly affects minority populations (such as ethnic minorities and low income individuals), because of substandard housing and indoor air quality, and because health education may not be culturally relevant or account for lower levels of literacy. There is also variable adherence to guidelines amongst providers, especially in terms of carrying out allergy testing and developing asthma action plans. A lack of patient centeredness and poor communication between patient and provider also contribute to low adherence and health inequities.

Dr Stout and the Guidelines to Practice (G2P) group are addressing these issues through a community based participatory research project. The study was designed with input from a consortium of patients, public health organisations and experts in health information and quality improvement. The concept behind this project came from an earlier demonstration project funded initially by the American Lung Association of Washington in 1995, in which the team developed an Asthma Outreach Project at Odessa Brown Children’s Clinic, involving home visits and planned clinic visits using an asthma Community Health Worker model. The Asthma Outreach Project at Odessa Brown was a proof of concept, further developed, refined and evaluated through a series of studies, conducted primarily by researchers led by Dr Jim Krieger at Seattle/ King Country Health Department over two decades.
Firstly, the G2P project aimed to improve the implementation of asthma guidelines through integrated multicomponent interventions. Key recommendations of these guidelines include making a correct diagnosis, assessing asthma severity and control, integrating spirometry testing and allergy skin prick testing into usual work flow for planned asthma visits, appropriately prescribing medications and providing and using an Asthma Action Plan. During the study, participants were randomly assigned into four groups: with or without the services of a Community Health Worker (CHW), and with or without services at a practice receiving specialised training in delivering preventive asthma care. The group that the G2P team were most interested in focusing on was the one where CHW services were being integrated with the trained ‘intervention’ practices. For this group, the team built a preventive asthma template used as a communication portal between the CHW and the practice team, to integrate the work of each. Results of this trial will soon be available. ‘The real “innovation” of this trial was the development of this EHR portal, and its use by both CHWs and the practice,’ says Dr Stout. So what do each of these interventions involve? The health plan enhancement intervention comprises case management, increased passive guideline dissemination, medication fill monitoring and provider education. Case managers received training from asthma experts, while healthcare providers are notified of any hospitalisations or emergency department visits involving their patients within 24 hours of discharge.
The enhanced clinic intervention implements multiple components of decision support, audit and feedback, staff education and electronic health record (EHR) enhancements. Team based care is encouraged through integrated communication platforms and system redesign. Asthma champions helped to redesign the clinic team and system, while the Chronic Care Model Framework and continuous quality improvement activities are employed to provide enhanced pre-visit assessment, focused clinical encounters and expanded post-visit options.
Finally, community health worker home visits provide patients with tailored self-management plans to control their asthma. This allows the community health workers to work with patients and learn about their challenges and concerns, provide targeted education and referrals to resources and implement an individualised management plan. Trigger reduction in the home is supported through the provision of education and additional resources (such as allergen impermeable bedding and low emission vacuum cleaners).
The community health workers also have access to the integrated EHR platform in order to share information with the rest of the team. The G2P project is innovative in its development of a multicomponent, multi-level systems approach to asthma management. As well as the benefits to patients (better health and quality of life, better self-management skills and improved communication with health care providers), clinicians have gained tools to enhance their skills and patient relationships as well as a CHW serving as their ‘eyes and ears’ into the patient’s home environment. The G2P team also hope that the project will lead to improved quality metrics, decreased healthcare costs, and reduced health inequities. The potential of this project to improve asthma management is great and, if proven models like this are widely adapted, the future is bright for asthma sufferers worldwide.
Meet the Spirometry 360 Team
Dr Jim Stout
Dr Jim Stout is Professor of Paediatrics and Adjunct Professor of Health Services in the University of Washington. He is Founder and Director of Interactive Medical Training Resources (iMTR), whose ‘flagship’ program is Spirometry 360, at the Child Health Institute in Seattle. After completing his MD at the Bowman Gray School of Medicine, he went on to receive his paediatric residency training at University of Washington, and his MPH from the University of Washington School of Public Health. He served as Director of the Asthma Clinic in the Odessa Brown Children’s Clinic for over two decades. His research interests include asthma and office-based diagnostic spirometry, quality improvement and the development of remote physiological monitoring applications deployed through smartphones.
Dennis Burges
Dennis Burges is a software engineer who develops remote training web applications and produces audiovisual resources for distance learning platforms on a variety of health care topics.
Ben Hedrick
Ben Hedrick manages enrolment and the day-today operations of Spirometry 360. He also designs, implements, and monitors updates to course websites and online advertising and co-develops new online training programs.
Sharon Kiche
Sharon Kiche works on international projects where she tracks and manages communications and produces progress reports for member countries.
Drew Martenson RRT
Drew Martenson is a respiratory therapist and Chief Over-Reader for Spirometry 360. His central focus is the reading, grading, and education of Spirometric testing, and providing coaching insights and quality feedback to the practices that participate in the Spirometry 360 program.
Bonnie Rains
Bonnie Rains manages clinical and quality improvement projects and related activities.
Louise C. N. Warren MPH
Louise C. N. Warren provides research and program coordination, financial management, and organisational support for Dr Jim Stout and team.
Maria Hamilton
Maria Hamilton provides fiscal management support for Dr Jim Stout’s grants and other projects.
FUNDING
Agency for Healthcare Research and Quality (AHRQ)
Centers for Disease Control and Prevention (CDC)
CoMotion, University of Washington Coulter Family Foundation, University of Washington European Commission
International Primary Care Respiratory Group (IPCRG)
Life Sciences Discovery Fund, Washington State National Institutes of Health (NIH):
National Heart, Lung, and Blood Institute (NHLBI)
Patient Centered Outcomes Research Institute (PCORI)
CONTACT
www.spirometry360.org
imtr@uw.edu
jstout@uw.edu