Dr Afsaneh Lavasanifar – Improving Cancer Treatment with Nanomedicine
Cancer is one of the most common causes of mortality worldwide and diagnosis rates are continually increasing. An estimated one in three women and one in two men will be diagnosed with a form of cancer at some point throughout our lives. For many cancer types, chemotherapy and radiotherapy are the chosen treatment methods, but their success rates are surprisingly limited, and both can cause serious side-effects. Dr Afsaneh Lavasanifar and her research group at the University of Alberta have set out to develop drug-delivery systems to improve the effectiveness of cancer treatment and reduce side-effects. Their research involves the targeted delivery of drug-loaded nanoparticles directly to tumour tissues.
The Need for Better Cancer Treatment
With the number of cancer diagnoses on the rise, successful treatment is becoming increasingly essential. Whilst chemotherapy and radiotherapy are frequently used to treat cancer, they can be ineffective in many cases and are extremely harmful to healthy tissues, resulting in a variety of serious side-effects.
Chemotherapy involves administering multiple drugs into a patient’s bloodstream to destroy cancer cells. While such drugs have significant toxic effects in cancer cells, they are poorly specific for cancer and can also attack healthy tissue. Rather than exposing the patient’s entire body to these anti-cancer drugs, delivering them directly to tumour tissues can significantly improve treatment outcomes and reduce side-effects.
Likewise, radiotherapy involves a patient being exposed to large doses of radiation. While it can be effective in destroying tumour cells, it can also have a negative impact on healthy tissue. The use of supplementary drugs delivered specifically to tumours during radiotherapy can improve treatment efficacy and allows the radiotherapist to use smaller doses of radiation.
Dr Afsaneh Lavasanifar, of the University of Alberta in Canada, has focused her research on the development of nanoparticles for drug delivery that can provide safer and more efficient treatment for those diagnosed with cancer. ‘As a pharmacist by training, I have witnessed the adverse effects of medications in patients, first-hand,’ says Dr Lavasanifar. ‘In some cases, such as with anti-cancer chemotherapeutics, these side-effects are even more detrimental to the patient than the disease, itself, and significantly diminish the patient’s quality of life.’

Therapeutic Nanocarriers
Nanomedicine, a fast-evolving area of research, involves the use of therapeutic nanoparticles, and aims to improve on traditional drug administration techniques. Dr Lavasanifar and her team develop nanoparticles called ‘nanocarriers’ that can carry anti-cancer drugs to tumours to support cancer treatment, with the aim of increasing the specificity of such treatments for cancer cells. ‘We are trying to make drugs in general and anti-cancer drugs in particular work better and have fewer side effects by redirecting them from healthy organs and cells to diseased tissues,’ Dr Lavasanifar explains.
Nanocarriers are very small particles that can encapsulate other molecules, such as anti-cancer drugs, and transport them throughout the body. The use of nanocarriers for delivering drugs can sometimes be essential, such as when a drug is too delicate or insoluble to persist in the bloodstream on its own. Nanocarriers also make it easier to direct drugs to specific organs or tissues.
Dr Lavasanifar and her colleagues utilise ‘micelles’ as nanocarriers to encapsulate anti-cancer drugs. Micelles are tiny molecules no larger than 200 nm, which have a hydrophobic (water-repelling) core and a hydrophilic (water-attracting) shell. Their core can host different compounds and their shell allows them to be transported throughout the body without being detected by the immune system.
Dr Lavasanifar and her team chose these micelles because of their ability to encapsulate drugs that are insoluble in water and therefore cannot be administered into the bloodstream on their own. They are also safe for human administration as they are both biocompatible and biodegradable and can be excreted through the kidneys after they are no longer needed in the body.
Importantly, micelles also allow for passive tumour targeting, whereby they will preferentially accumulate in tumour tissues because of the leaky nature of tumour blood vessels. The small size of the micelles allows them to pass through small holes in these blood vessels, and they then accumulate in tumours, in a process known as the enhanced permeability and retention effect. As healthy tissues contain non-leaky blood vessels, the micelles do not tend to accumulate in such tissues.
In 2006, Dr Lavasanifar and her team developed new micellar carriers and showed that they are more effective nanocarriers for the transportation of a variety of drug molecules. These newly developed nanocarriers have the potential to be modified to increase their clinical usefulness These improvements include increased stability of the micelles, so that they can persist for longer in the body, while allowing more drug to accumulate in the target tumour.
This project provided the catalyst for further research by the team, utilising these micelle nanocarriers for the delivery of specific anti-cancer compounds.
‘The use of nanomedicine for new anti-cancer agents can prove to be a viable approach in bringing more new drugs with improved activity and reduced side-effects to clinical use.’

Active Targeting and Tracing
Dr Lavasanifar and her colleagues have also attached molecules to the surfaces of micelles that further facilitate their accumulation in tumours. In one recent study, the team attached a cancer-targeting molecule to two different types of micelles. This protein molecule can bind to other proteins that tend to be highly concentrated on the surfaces of breast cancer cells, thereby helping the micelle deliver its contents to the cancer cell.
Although this technique is highly advanced, the team found that the stability of the micelles had a greater impact on increasing accumulation in tumour tissue in a rat model, through ‘passive tumour targeting’, compared to attaching cancer-targeting molecules to the micelles.
The researchers confirmed the exceptional targeting ability of their micelles for tumours by tracking their location as they moved through the bodies of mice. The team was able to do this by incorporating dye molecules or contrast agents into their micelles, allowing them to be detected using imaging techniques.
This ability to trace nanocarriers after they are administered into the body can allow researchers to monitor their distribution and assess their usefulness in cancer treatments, while also ensuring their safety.
Overcoming Multidrug Resistance
Multidrug resistance (MDR) occurs when a tumour stops responding to treatment and can occur at any stage during a course of chemotherapy. It is thought to happen as a result of tumours eliminating or deactivating chemotherapy drugs, thereby protecting cancer cells from destruction.
Preventing MDR would greatly improve the chances of a given cancer treatment being successful. However, molecules that can inhibit the mechanisms tumours use to eliminate chemotherapy drugs lack specificity for cancer cells and can cause side-effects in healthy tissues, or make healthy cells sensitive to the effect of chemotherapy drugs. Because of this, such ‘MDR inhibitors’ have failed to achieve clinical approval to date.
A nanocarrier delivery system capable of achieving targeted delivery of these inhibitors would greatly enhance the treatment of MDR cancers. Such a nanocarrier would need to overcome the current limitations of MDR inhibitors, such as their poor stability, low cellular uptake, and rapid clearance from the bloodstream.
As part of their research into micelle nanocarriers, Dr Lavasanifar and her group have successfully shown that a chemotherapy drug and an MDR inhibitor can be encapsulated together within their micelles, for co-delivery to a tumour. In addition to relying on passive targeting, molecules attached to the surfaces of the micelles that bind to cancer cells ensure greater accumulation at the tumour site.

Inhibiting DNA Repair Systems
Cancer cells are often extremely good at repairing the damage caused by chemotherapy and radiotherapy, and contain molecules that recognise and repair DNA breakages, negating the effects of many cancer treatments. Inhibiting these DNA-repair molecules from operating in tumour tissue improves the cancer’s sensitivity to therapy. Likewise, it is also essential that these inhibitors accumulate in tumour tissue only, to allow healthy cells to continue the essential repair of damaged DNA.
After their success in delivering drugs to MDR cancer cells, Dr Lavasanifar and her colleagues used their micelle nanocarriers to encapsulate and deliver DNA-repair inhibitors to improve the sensitivity of colorectal cancers to treatment. Again, they improved the selectivity of these micelle nanocarriers by attaching molecules to their surfaces that specifically bind to molecules present on colorectal cancer cells. Furthermore, these micelles were no larger than 100 nm, allowing for substantial uptake and accumulation in tumour tissue. The group successfully demonstrated the targeted delivery of these micelle nanocarriers and the release of their therapeutic payload in colorectal cancers in mice.
Hydrogels for Drug Delivery
Dr Lavasanifar and her collaborators have also developed a ‘hydrogel’ formulation (called PolyGelTM) from the same safe building blocks as their micelles. Drugs can be loaded into this substance, and it can then be applied to the skin or injected into tissues, where it can release of a variety of drugs gradually.
PolyGel is a liquid at room temperature and forms a gel at body temperature. This formulation provides high stability and may be useful for a wide range of therapeutics. Dr Lavasanifar and her team have tested the hydrogel in animal models for the delivery of drugs to the surface of the eye and topical treatments for skin cancer treatment.
Future Directions
Overall Dr Lavasanifar’s research has provided essential contributions to the field of nanomedicine. Specifically, this body of work has involved improving cancer treatments through the development of traceable micelle-based delivery systems that show excellent tumour-targeting ability.
‘The use of nanomedicine for new anti-cancer agents can prove to be a viable approach in bringing more new drugs with improved activity and reduced side-effects to clinical use,’ says Dr Lavasanifar. Towards this aim, her team is currently carrying out research to improve lung cancer treatment using micelles to prevent DNA repair in tumour cells. ‘We are expediting the advancement of this new form of anti-cancer therapy in preclinical research.’ The clinical use of these nanocarriers will undoubtedly have an overwhelmingly positive impact on the prognosis and quality of life for many patients in the future.
Reference
https://doi.org/10.33548/SCIENTIA505
Meet the researcher

Dr Afsaneh Lavasanifar
Department of Pharmacy and Pharmaceutical Sciences
University of Alberta
Edmonton, Alberta
Canada
Dr Afsaneh Lavasanifar gained her PhD from the University of Alberta in 2001, where she is now a Professor in the Faculty of Pharmacy and Pharmaceutical Sciences with a joint appointment in the Department of Chemical and Material Engineering. Her research encompasses the development of drug delivery systems to enhance therapeutics, with a specific focus on nanomedicine to improve cancer treatment. In addition to her academic research, Dr Lavasanifar holds numerous patents and is also the Scientific Chief Officer and Vice President of a spinoff company called ‘Meros Polymers’, which is founded on the technology developed by her lab. She is also the Associate Editor of Molecular Pharmaceutics, and a member of the editorial board for Materials Sciences and Applications. Dr Lavasanifar has received many awards and honors during her career, including the TEC Edmonton Innovation Makes Sense Award in 2013 and 2016, the Sanofi-Aventis/AFPC New Investigator Award in 2009 and the GSK CSPS Early Career Award in 2007 in recognition of her outstanding research in pharmacy.
CONTACT
E: afsaneh@ualberta.ca
W: https://www.ualberta.ca/pharmacy/about-us/contact-us-and-people/people/afsaneh-lavasanifar
KEY COLLABORATORS
Dr Michael Weinfeld
Dr Dennis Hall
Dr Hasan Uludag
Dr Kamaljit Kaur
Dr Frank Wuest
FUNDING
Natural Science and Engineering Council of Canada (NSERC)
Canadian Institute of Health Research (CIHR)
Canadian Foundation for Innovation (CFI)
Alberta Innovates Health Solutions (AIHS)
Alberta Cancer Foundation (ACF)
FURTHER READING
Z Shire, MR Vakili, TDR Morgan, DG Hall, A Lavasanifar and M Weinfeld, Nanoencapsulation of novel inhibitors of PNKP for selective sensitization to ionizing radiation and irinotecan and induction of synthetic lethality, Molecular Pharmaceutics, 2018, 15, 2316.
SM Garg, IM Paiva, MR Vakili, R Soudy, K Agopsowicz, AH Soleimani, M Hitt, K Kaur and A Lavasanifar, Traceable PEO-poly(ester) micelles for breast cancer targeting: The effect of core structure and targeting peptide on micellar tumor accumulation, Biomaterials, 2017, 144, 17.
XB Xiong and A Lavasanifar, Traceable multifunctional micellar nanocarriers for cancer-targeted co-delivery of MDR-1 siRNA and Doxorubicin, American Chemical Society, 2011, 5, 5202.
A Mahmud, XB Xiong and A Lavasanifar, Novel self-associating poly(ethylene oxide)-lock-poly(ϵ-caprolactone) block copolymers with functional side groups on the polyester block for drug delivery, Macromolecules, 2006, 39, 9419.

Creative Commons Licence
(CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
More articles you may like
Calculating Steering Friction: Essential Engineering for Military Aircraft Safety
The safe operation of military training aircraft depends on precise engineering calculations that most of us never consider. Dr Bogdan Adrian Nicolin and Dr Ilie Nicolin from the National Institute for Aerospace Research in Romania have developed sophisticated methods to calculate the steering friction moment in military aircraft. This critical engineering parameter ensures that pilots can safely control aircraft during taxiing, take-off, and landing – making their work essential for both pilot training and flight safety.
Professor Robert B Heimann | Culinary Craftmanship: The Evolution of Pottery for Cooking
Cooking food is arguably one of the most important transitions in human evolution, and initiated hundreds of thousands of years of refinement in both technique and technology. Professor Emeritus Robert B Heimann of TU Bergakademie Freiberg, Germany, recently reviewed the evidence for early cooking vessels and tracks the evolution of their production, identifying important strategies of optimisation using various natural materials, firing methods, and designs to improve durability, functionality, and efficiency over time.
Dr Loren Babcock | Untangling the History of Jefferson’s Giant Ground Sloth
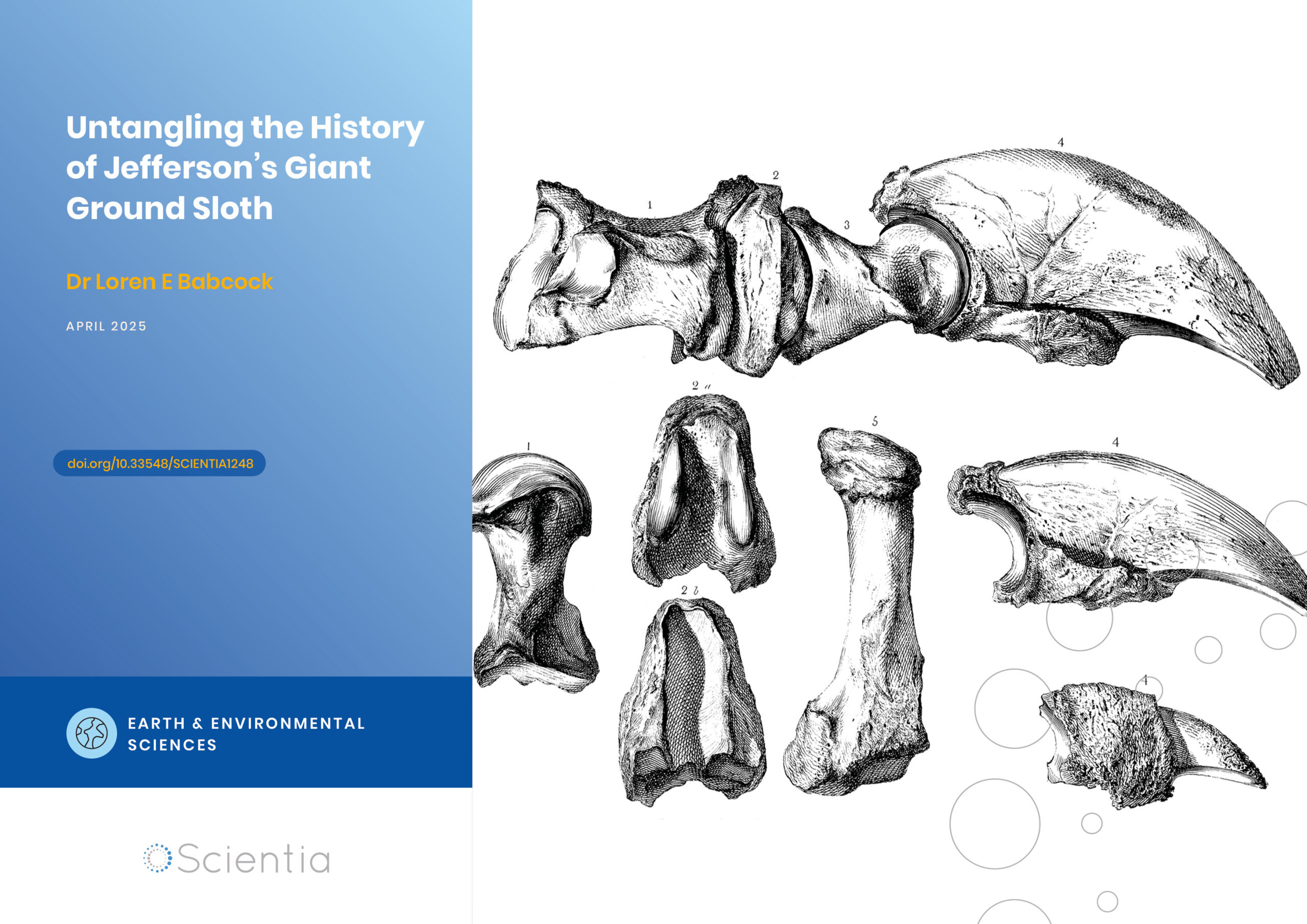
In the spring of 1796, workers mining saltpetre in a western Virginia cave unearthed several unusual bones. This would launch the scientific study of extinct animals in North America and connect one of America’s founding fathers to the early development of palaeontology. Some of these mysterious bones eventually made their way to future US President Thomas Jefferson at his Monticello estate. Dr Loren Babcock from The Ohio State University’s School of Earth Sciences has conducted an extensive review of the complex naming history of this iconic extinct animal. His research untangles over 200 years of inconsistent scientific terminology and establishes the definitive nomenclatural history of what would become known as Megalonyx jeffersonii.
Epigenetic Mysteries Unravelled: The Zinc-Finger Proteins
Exploring the complex mechanisms of cell development processes and DNA structure is critical to understanding how certain diseases, such as cancer, can arise. Professor Danny Reinberg and Dr Havva Ortabozkoyun from the University of Miami in Florida, USA, work to reveal the epigenetic mechanisms at play during cell division and development and, in turn, disease processes. Together, they are discovering new protein molecules involved in genome organisation, deepening our understanding of how cancers and other related conditions can develop.