Dr Simon Graham – Making Magnetic Resonance Imaging Examinations Safer for Patients with Deep Brain Stimulation Implants
Deep brain stimulation (DBS) is an increasingly popular treatment for abnormal brain circuits found in epilepsy, obsessive-compulsive disorder, Parkinson’s disease and other conditions. Magnetic resonance imaging (MRI) examinations are part of the medical workup to implant DBS devices correctly, and can be used after the procedure to assess potential complications, provide long-term follow-up or evaluate new disease. At present, however, MRI of patients with DBS implants may introduce a significant risk of heating brain tissue. Dr Simon Graham, at the Sunnybrook Research Institute in Toronto, investigates how MRI can be optimised to keep DBS patients safe.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is used to create images of the soft tissues inside the body. Detailed MRI examinations are now an essential tool in medicine, assisting in the diagnosis and treatment of many ailments such as strokes, infections and tumours.
Powerful magnets are the main component of MRI machines. When a patient lies inside, the magnet pulls on the magnetic fields of protons in all of the hydrogen atoms in the patient, forcing the protons towards magnetic alignment. This alignment is then knocked out of order by transmitting short bursts of radiofrequency (RF) electromagnetic waves into the patient. Once the RF transmission stops, the protons return to their previous alignment and release RF signals which are then read by the MRI machine. During imaging, other magnetic fields that vary linearly with position, and aspects of the RF transmission are manipulated so that the received MRI signals are ‘spatially encoded’. Physicians are then able to distinguish between normal tissues, and between normal and diseased tissues, based on MRI signal location and signal strength.
The MRI signals are primarily received by water and fat molecules and have different signal strengths in different tissues for many reasons. Variations in tissue water and fat content play a role; another contributing factor is that protons realign at varying speeds according to the different molecular and microstructural environments in each type of tissue. Because MRI signals have diverse properties, many different types of images can be created for various medical purposes.
Functional Magnetic Resonance Imaging
As just mentioned, there are many different imaging techniques in the ‘MRI portfolio’. Beyond images of anatomy, a technique called functional magnetic resonance imaging (fMRI) looks into the function of neural tissue in the brain and spinal cord. When a region of the brain becomes active during mental processing, increased blood flow, blood volume and blood oxygenation are supplied to the region as part of supporting the energy demands of cells. Most fMRI exploits this effect by measuring blood oxygen level-dependent (BOLD) signals, to produce colour-coded images that depict the strength of activity across the brain.
When performed during an appropriate behavioural task (or increasingly, when patients are at rest and thinking of nothing in particular) fMRI can be used to determine sites of activation supporting brain functions such as memory, movement and language. These data can then be taken into account before brain surgery, for example, to give a surgeon guidance on the areas that should be avoided to minimise behavioural side effects.

Deep Brain Stimulation
Implanting electrodes into the brain may seem extreme, but in fact, it is an increasingly common approach when other treatment options, like drugs, do not work or become ineffective for various diseases. Deep brain stimulation (DBS) involves neurosurgery to implant a thin wire lead tipped with electrodes into the brain. Alternatively, two wires can be inserted to target similar structures on each side of the brain.
To ensure that the electrodes are placed correctly and precisely, patients undergo MRI before their operation so that the surgeons can see the patient’s specific brain structure and identify the treatment targets. Incredibly, patients are usually not fully sedated when the DBS device is implanted. A local anaesthetic may be given to block pain during the opening of the skin and drilling through the skull. However, the brain contains no nerve endings and pain cannot be felt there, enabling most patients to remain awake so that the surgeon can monitor their behavioural signs during insertion of the lead and electrodes. Afterwards, the remaining extent of the lead (or leads) is then run under the skin and attached to a battery-powered pulse generator implanted near the collarbone.
After successful surgery, electrical impulses are delivered to the brain to regulate the abnormal neural activity resulting from disease. As the pulse generator is adjusted by remote control, the patient and their doctor can manage and program it easily from outside the body. The amount and timings of stimulation depend on the patient’s condition – DBS may only be necessary during the day, for example, or it may be constant.
A person may try DBS for very many reasons. Parkinson’s disease, epilepsy, obsessive-compulsive disorder, and a common movement disorder called essential tremor are some of the most common conditions that are treated by DBS, but its usefulness for other diseases is being investigated too. For example, DBS holds early promise for Tourette syndrome, addiction, major depression and multiple sclerosis.
However, there is a specific issue that arises when DBS and MRI are combined, and this is the focus of Dr Simon Graham’s research at the Sunnybrook Research Institute in Toronto.

The Risk of Magnetic Resonance Imaging after Deep Brain Stimulation
An MRI examination is completed before a DBS operation but is also useful afterwards. This is because any side effects of the treatment can be examined, the implant location can be checked, and a patient’s health can be monitored over the long term. Functional MRI may also be useful to assess the patient’s brain activity and see whether it becomes more normal, or as part of research trials to investigate more about how DBS treatments work, toward optimising DBS device technology. Together with fMRI, another technique called diffusion weighted imaging may be useful to identify how different brain regions are connected – to verify the neural network under treatment, and whether other networks are being stimulated in error, potentially with behavioural side effects.
A more powerful MRI machine is becoming increasingly available, producing better quality images than before. It generates a magnetic field of 3 Tesla (T), which means that it is twice as strong as previous machines that operated at 1.5 T. These 3T MRI machines are great for pre-operative imaging of DBS patients because the electrodes can be placed even more accurately.
However, MRI is a possible safety risk for patients with DBS implants, especially when 3T machines are used. The main concern is that current may be induced in the metal leads of DBS devices during the RF transmission portion of MRI. The leads carry this unwanted current to the electrodes, which then potentially heat and damage the brain tissue surrounding the wire. Temperature increases from 1 degree Celsius to as high as 46 degrees have been found, depending on various factors including magnetic field strength and the type of ‘coil’ hardware used for RF transmission. Damage to tissue in the brain could have serious consequences, so this heat effect presents too big of a risk for most patients to receive an MRI following a DBS implant.
While there are some exceptions where specific ‘MRI-conditional’ DBS devices can be imaged, these are under very conservative conditions that reduce image quality and DBS capabilities during imaging. Dr Graham and his team are investigating how to overcome this state of affairs, and uncover how MRI can be carried out more safely for patients with DBS implants.

Tailoring Radiofrequency Transmission
Two main avenues for improving safety have been explored by researchers: revising the design and materials of DBS devices, and modifying RF transmission. Dr Graham investigates the latter in his work, using a technique called parallel radiofrequency transmission (pTx). Instead of a single coil surrounding the patient for RF transmission, pTx utilises multiple coils that can be independently coordinated and powered. As a result, the distribution and strength of the RF magnetic fields can be controlled to maintain image quality, while also manipulating the RF electric field to minimise localised power deposition and tissue heating from the DBS device.
Dr Graham’s team wanted to confirm the efficacy of using pTx during MRI in their initial study published in 2015, and they found that it did, in fact, reduce localised power deposition and tissue heating, due to a 95–99% reduction in the local RF electric field. The team used electromagnetic simulations for their tests. They studied how the number of RF transmitter coil elements affected homogeneity (the ability to generate a uniform image) while suppressing localised heating in a uniform, cylindrical, tissue-equivalent medium containing an implanted wire. Two, four and eight elements were tested and the team noted that although more investigations would be needed, the results with four elements were very promising.
Building on the Findings
Further studies in 2017 and 2019 allowed Dr Graham and his team to continue developing how pTx can be incorporated in MRI to give the best outcomes for DBS patients. Preliminary studies had used DBS leads with extremely simplified trajectories. In real-world scenarios, however, the leads can have complex geometries. Excess lead length is often placed in overlapping loops at the surface of the skull, and the lead configuration ultimately differs from person to person due to various factors including the shape of the head, the type of disease and the clinical symptoms displayed. The variability in DBS lead trajectories should not be overlooked, as it can have a major influence on the extent that tissue heating occurs near the electrodes. Therefore, Dr Graham and his team wanted to research heat-reduction methods such as pTx in realistic patient-specific situations. They also improved on their previous simulations to make the study more relevant to the real world. For example, they introduced insulated wires with conductive ‘electrode’ ends, rather than perfectly conducting wires, and validated simulation results using custom-built four-element pTx hardware that was much more advanced.
The improved variables and calculations gave promising results. Localised power deposition around the electrode was impressively reduced by 94% when using four-element pTx and 97% when using eight-element pTx. When their optimised results were tested experimentally on a realistic model, called a head phantom, they generated good-quality images with four-element pTx while finding almost no temperature rise surrounding the tip of the wire.

Promising Results for Real-world Applications
Dr Graham and his team of dedicated researchers have delved into the topic of parallel RF transmission and provided optimised data that can be used in the future to minimise temperature rises in the brains of DBS patients receiving MRI. His work will contribute towards drastically reducing the risks for people receiving this treatment, and may prevent life-altering brain injuries. Combined with his additional work on brain activity, disease and MRI investigations, Dr Graham continues to make innovative contributions to his field.
Reference
https://doi.org/10.33548/SCIENTIA708
Meet the researcher

Dr Simon J. Graham
Sunnybrook Research Institute
Sunnybrook Health Sciences Centre Toronto
Ontario Canada
Dr Simon Graham obtained his B App Sc (Hons) in Engineering Physics in 1988 from Queen’s University in Ontario, Canada. He then went on to achieve a PhD in Medical Biophysics in 1995 from the University of Toronto, also in Canada. Having undertaken numerous research roles, he now works at Sunnybrook Research Institute as a Senior Scientist and Academic Director of research MRI facilities, as well as holding a professorship in the Department of Medical Biophysics at the University of Toronto. Dr Graham’s work focuses on developing MRI technology to facilitate better diagnosis and treatment for patients with diseases in the brain, especially involving fMRI to record brain activity. With over 165 papers published in scientific journals and over 12,000 citations as reported by Google Scholar (July 2021), Dr Graham’s work has a high impact in his field.
CONTACT
E: sgraham@sri.utoronto.ca
W: https://sunnybrook.ca/research/team/member.asp?t=11&m=487&page=528
Twitter: @SimonJGraham1
KEY COLLABORATORS
Dr Tom A Schweizer, Keenan Research Centre for Biomedical Sciences, St. Michael’s Hospital, Toronto
Dr Nir Lipsman, Harquail Centre for Neuromodulation, Sunnybrook Health Sciences Centre, Toronto
Dr Clement Hamani, Sunnybrook Research Institute, Sunnybrook Health Sciences Centre, Toronto
Dr Sanjay Kalra, Department of Medicine, Division of Neurology, University of Alberta, Edmonton
FUNDING
The Canadian Institutes of Health Research (CIHR)
The Natural Sciences and Engineering Research Council (NSERC) of Canada
The Canadian Foundation for Innovation
Mitacs
FURTHER READING
M Arianpouya, B Yang, F Tam, et al., Safe MRI of Deep Brain Stimulation Implants: A Review of the Promises and Challenges, Frontiers in Neurology and Neuroscience Research, 2, 100012.
Z Lin, F Tam, NW Churchill, et al., Tablet Technology for Writing and Drawing during Functional Magnetic Resonance Imaging: A Review, Sensors, 2021, 21(2), 401.
B Davidson, F Tam, B Yang, et al., Three-Tesla Magnetic Resonance Imaging of Patients with Deep Brain Stimulators: Results From a Phantom Study and a Pilot Study in Patients, Neurosurgery, 2021, 88(2), 349–355.
S Kalra, HP Muller, A Ishaque et al., A Prospective Harmonized Multicenter DTI Study of Cerebral White Matter Degeneration in ALS, Neurology, 2020, 95(8), e943-e952.
CE McElcheran, L Golestanirad, MI Iacono, et al., Numerical Simulations of Realistic Lead Trajectories and an Experimental Verification Support the Efficacy of Parallel Radiofrequency Transmission to Reduce Heating of Deep Brain Stimulation Implants during MRI, Scientific Reports, 2019, 9, 2124.
CE McElcheran, B Yang, KJT Anderson, et al., Parallel Radiofrequency Transmission at 3 Tesla to Improve Safety in Bilateral Implanted Wires in a Heterogeneous Model, Magnetic Resonance in Medicine, 2017, 78(6), 2406–2415.
CE McElcheran, B Yang, KJT Anderson, et al., Investigation of Parallel Radiofrequency Transmission for the Reduction of Heating in Long Conductive Leads in 3 Tesla Magnetic Resonance Imaging, PLoS One, 2015, 10, e0134379.
Want to republish our articles?
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence
(CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
More articles you may like
International Isocyanate Institute | TDI-induced Asthma: Reanalysing Data to Find Hidden Trends
Even if you’ve never heard of them, you’ve used polyurethanes. Producing them requires toluene diisocyanates, which may/can induce asthma when inhaled. A 5-year study claimed to conclude that cumulative TDI exposure over time was indicative of asthma incidence. However, a reanalysis by a team at the International Isocyanate Institute points the finger instead at the frequency of unprotected high-exposure events, like accidental spills or plant maintenance. This finding guides the way for future advances in worker safety.
A New Way to Detect and Identify Forensic Bloodstains
Accurately identifying bodily fluids at crime scenes is vital to aid forensic examinations and obtain information for use in criminal proceedings. However, collecting viable material for analysis can be challenging, especially if samples are difficult to access or the amount is minute. Dr Lamyaa Almehmadi and Professor Igor K Lednev at the University at Albany, State University of New York, USA, have introduced a new technique to assist in analysing bloodstains for forensic examination without compromising sample integrity.
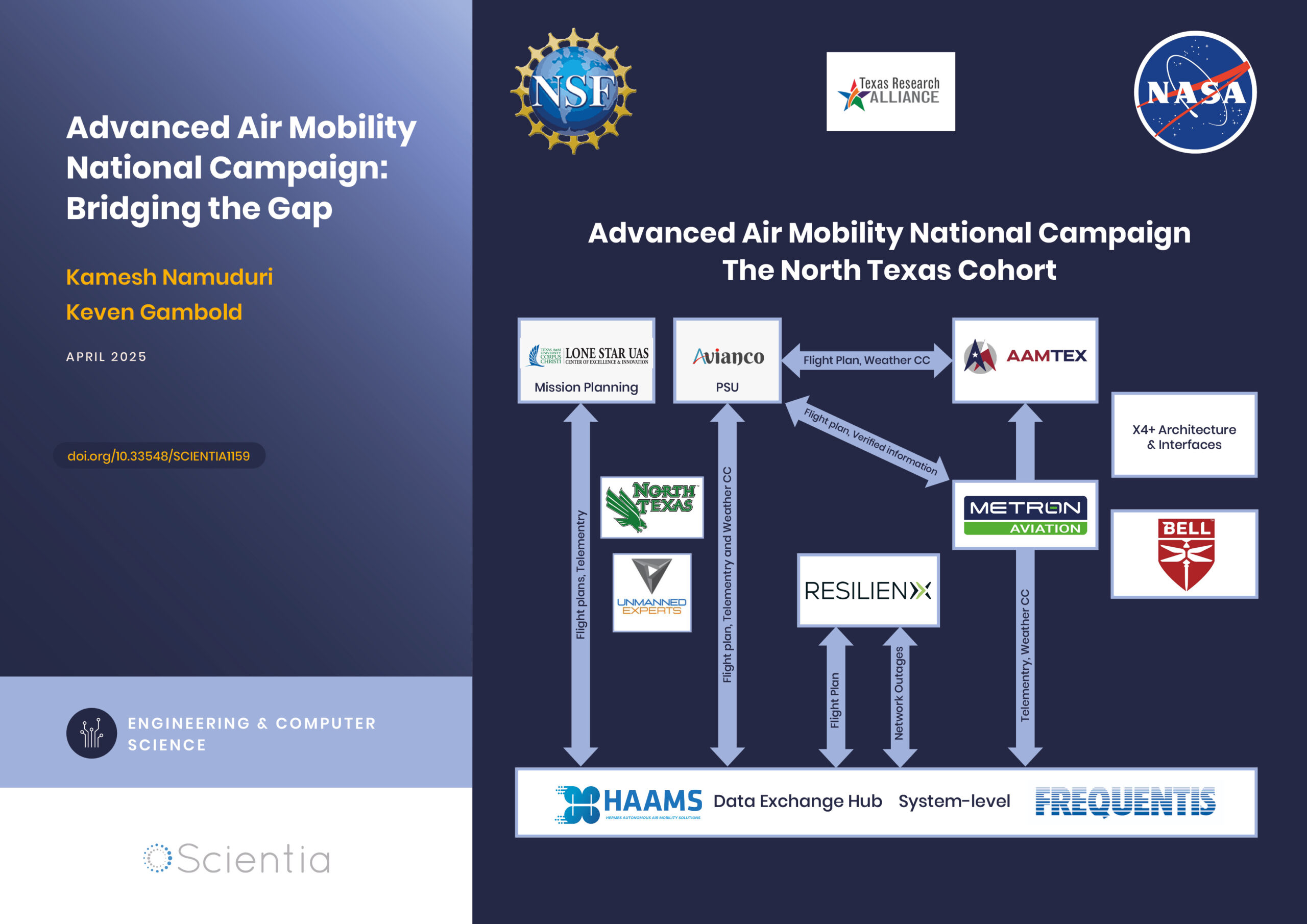
Advanced Air Mobility National Campaign: Bridging the Gap
The rapid advancements in technology have paved the way for revolutionary changes in transportation, particularly air mobility. One such groundbreaking initiative is the Advanced Air Mobility (AAM) National Campaign led by NASA. This campaign aims to integrate advanced air mobility solutions into the existing transportation infrastructure, creating a seamless, efficient, and safe urban air transportation system. By addressing the various challenges associated with urban air mobility, the AAM National Campaign is poised to redefine how we navigate our cities, ultimately leading to reduced congestion, improved accessibility, and enhanced environmental sustainability.
Dr Niloofar Vardian | Mapping the Unknown: Inside Black Holes
Dr Niloofar Vardian at the SISSA school has advanced our understanding of black hole interiors through precise mathematical modelling. Her recent publication sheds light on previously inaccessible aspects of black hole dynamics, deepening our knowledge of these mysterious and difficult-to-study phenomena.