Dr Susmita Bose | 3D Printed Bone-like Materials for Delivering Natural Medicine
Medical Materials
Thanks to modern medicine, people can expect to live longer, healthier lives than previous generations. This is wonderful, but increased life expectancy means that people may encounter more medical problems as they age, such as bone degradation. Bone can also be damaged due to trauma, disease, and birth defects, reducing the quality of life for millions of people worldwide.
In some cases, replacing damaged joints with mechanical prostheses can allow people to live full lives. In other cases, certain substances can be implanted into the site of the damaged bone, providing structural support and encouraging the growth of natural bone tissue. These procedures require cutting-edge materials in order to be successful.
Scientists work hard to develop these materials, which must be completely non-toxic and not be rejected by the body’s immune system. Mechanically, they need to mimic the physical properties of natural bone and should be strong enough to support patients in their daily activities. In the case of total joint replacements, the constituent materials must be durable and biocompatible enough to last for the rest of the patient’s life. Dr Susmita Bose and her team at Washington State University have been focusing their research efforts on developing and optimising bone-like materials to improve the quality of life for those with damaged bones and those who need joint replacements.
‘Whether it’s due to longer life expectancy, sports injuries, or a desire for a more active lifestyle in today’s world, we will need more bone replacement materials. And whether it is hip and knee replacements or fracture care, we will need replacement materials with a longer lifetime,’ says Dr Bose. ‘In some cases, patient-matched devices are necessary for patients with special anatomical needs or concerns related to specific defect size complexity. The role of 3D printing is becoming essential in those cases of patient-matched implants due to lower cost and shorter lead time to manufacture.’

Dr Susmita Bose with her graduate student Connor A. Toulou.
Creating Bone-like Materials and Structures Using 3D Printing
One of the prevailing issues with creating suitable materials for bone repair and joint replacement is making sure that they can be successfully integrated into the body. If a material is rejected by the body’s immune system, it can lead to complications, ultimately leaving the patient in a worse position following the operation.
Usually, prosthetic joints are made from metals, including titanium. Unfortunately, such implants often fail within 12 years, primarily because such metals are foreign to the human body. Additionally, because metal and bone have such different physical and chemical properties, implants cannot strongly bond to the surrounding tissues.
To solve this problem, Dr Bose and her team have been developing materials that can mimic the natural structure of human bone. Their aim is to use these materials both as a coating for metal-based implants, and as scaffolds that can be added to regions of damaged bone, to provide support and encourage the natural healing process.
The team’s new materials not only needed to have the same porous structure of bone, but they also needed to promote the growth of new cells. To create them, the researchers used a cutting approach: 3D printing technology. This process, which has become increasingly popular over the last decade, allows the user to produce a solid 3D structure based on a digital design. By adapting a 3D printer, the team was able to produce materials with a porous structure very similar to that of bone. In addition, the technique would enable a clinician to fabricate an implant with the exact shape and size needed to fit within a specific area of damaged bone.
‘You can use a bone-like ceramic powder as a feed material, and it can make whatever you draw on the computer,’ says Dr Bose. The feed material they used was based on calcium phosphate – a substance that partially mimics the properties of bone. When tested, the team’s 3D-printed scaffold materials showed far better cell adhesion than state-of-the-art bone repair materials, and also promoted the growth of new bone cells.
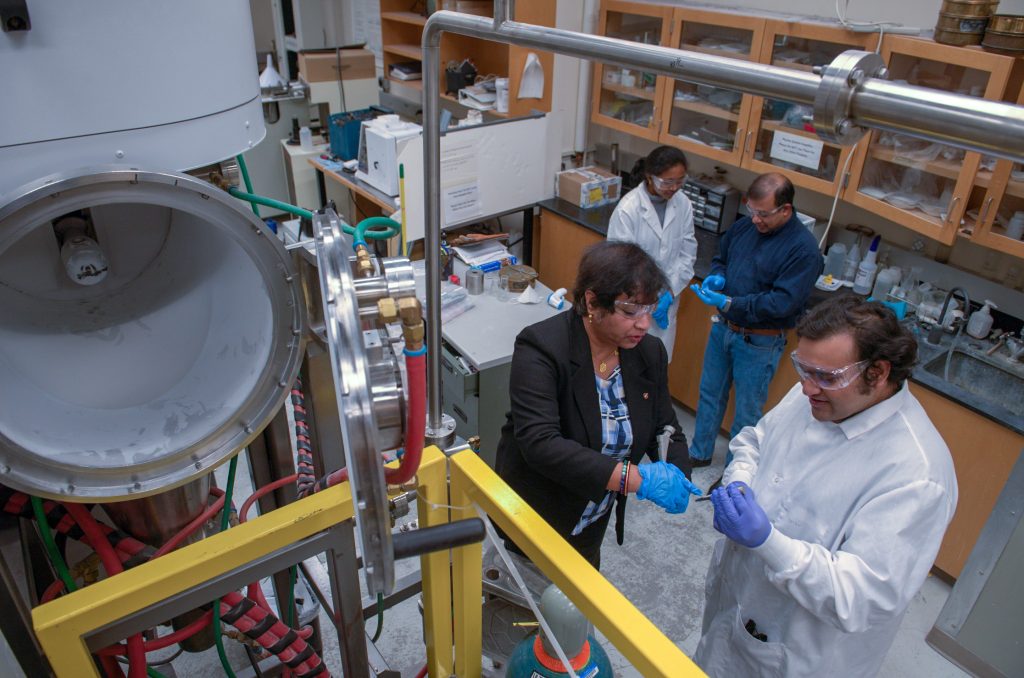
Dr Susmita Bose with her graduate student Ujjayan Majumdar
Delivering Therapeutic Compounds Through Bone Implants
Osteoporosis is a condition that affects millions of people worldwide and can cause significant issues related to bone fragility, which can lead to a higher likelihood of fractures, among other painful complications. Globally, more than 8.9 million fractures occur every year due to osteoporosis. There are several known causes of osteoporosis, the most common being deficiencies of vitamin D and calcium.
It is well established that vitamin D, specifically vitamin D3 , can promote bone health and encourage repair. However, it is not fully understood how the vitamin actually interacts with bone cells. Dr Bose and her colleagues wanted to close this gap in our knowledge, in order to better understand how this vitamin can benefit our bones, and help to combat conditions such as osteoporosis.
Furthermore, the team wanted to see how the calcium phosphate bone scaffolds that they had previously developed could be used to deliver vitamin D directly to damaged regions of bone. In theory, if a scaffold could be impregnated with vitamin D3 and implanted into the site of damaged bone, then it could release it gradually over time to promote bone healing, speeding up patient recovery.
Dr Bose and her colleagues began to investigate this idea by loading the vitamin into a polymer called PEG, which is commonly used for drug delivery. The team added this mixture to bone cells in dishes, in order to assess its potential effects on bone tissue. Through this experiment, the researchers found that the presence of vitamin D3 reduced the amount of breakdown observed in the bone cells. This suggests that the vitamin can help reduce bone mass loss and may be effective in helping to improve bone health, especially after an operation.
The team then loaded mixtures of vitamin D3 and polymers into samples of their artificial bone scaffolds, and monitored the release of the vitamin. From this, they gathered valuable data showing that the scaffolds gradually release vitamin D3 over time. They also found that the speed of its release is somewhat controlled by the type of polymer with which the vitamin is mixed before loading it into the scaffold. This was a significant breakthrough, demonstrating how the team’s bone-like scaffolds could represent tuneable and effective drug delivery systems, allowing for localised treatment of damaged bone.
Encouraging Bone Repair with Turmeric
In another recent study, Dr Bose and her colleagues investigated the potential of curcumin – the main component found in the spice turmeric – as a treatment for encouraging bone repair following surgery.
In many Asian countries, turmeric has been used as medicine for centuries, and recent research has indicated that curcumin has antioxidant, anti-cancer, anti-inflammatory, and bone-building properties. However, when consumed orally, curcumin is not absorbed very efficiently by the body, as it is not soluble in water. Therefore, to maximise its potential, an innovative method of drug delivery is required.
Just like in their vitamin D study, the team tested the ability of their calcium phosphate scaffolds to release curcumin. They did this by mixing the compound with various polymers, injecting the mixture into artificial bone scaffolds, and investigating the way in which it was released. Through this, the team was able to tune their polymer mixtures to give different rates of curcumin release.
This work could be particularly promising for patients with bone cancer. The team’s curcumin-loaded scaffold could potentially be applied to the area where a bone tumour was surgically removed. Not only would the scaffold and curcumin facilitate bone regeneration, but the anti-cancer effects of curcumin could also destroy any remaining tumour cells.

Dr Bose with her collaborators Professor Amit Bandyopadhyay and graduate student Priya Kushram.
Optimising Curcumin Delivery
As mentioned, curcumin is not soluble in water, meaning that it is difficult for the body to absorb. Fortunately, there is a solution: curcumin likes to form bond with certain metal ions. Dr Bose decided to expand on her previous work by developing a complex containing curcumin bonded to zinc, which is far more water soluble than curcumin alone. This, combined with a bone scaffold impregnated with fluoride, made it even easier to deliver curcumin to the target location. The combination of curcumin, zinc and fluoride not only allowed for more successful delivery, but also demonstrated some antibacterial properties. This could help to make future bone implants less prone to infection, greatly improving patient outcomes.
Expanding the Medical Spice Rack
Turmeric is not the only spice that has natural healing properties. In a more recent study, Dr Bose and her team created and tested artificial bone implants loaded with both gingerol, found in ginger, and allicin, found in garlic.
In both cases, they found a significant improvement in the development of bone cells, particularly when the implants had been loaded with gingerol or a mixture of the two extracts. Even more interestingly, they found that while the two extracts both seemed to benefit bone development, they had slightly different mechanisms of action.
Expanding on this research, the team tested allicin with other types of artificial bone implants, in order to collect more data on how it is released inside the body. While gathering this data, the team also analysed the effects of garlic as an antibacterial agent. These antibacterial properties represent an extra benefit associated with using allicin in bone implants. Just like curcumin, allicin may help to make bone implants infection-resistant, improving the chances of successful recovery.
Bringing Innovation to Patients
‘The addition of natural medicinal compounds with 3D-printed patientspecific biomedical devices, especially with calcium phosphate-based ceramics, is unique and groundbreaking,’ says Dr Bose. Indeed, her team has made substantial breakthroughs – not only in the world of material engineering but also in clinical chemistry and biology. Through their work, they have demonstrated the applications for these unique bone-like materials, how they can be successfully implanted into patients, and how they can be used to administer therapeutic compounds that can speed up the recovery process.
‘We’re always pursuing the quest for innovation,’ Dr Bose concludes. ‘Although I believe it is difficult to mimic Mother Nature, we’re striving to apply science and engineering to tackle health-related issues that will help us progress as a society. I’ll be happy if one day our research and innovation has been delivered to the patient’s bedside and advances human health. There would be no bigger satisfaction than that.’
SHARE
DOWNLOAD E-BOOK
LISTEN TO THE AUDIO
REFERENCE
https://doi.org/10.33548/SCIENTIA846
MEET THE RESEARCHER

Dr Susmita Bose
School of Mechanical and Materials Engineering
Washington State University
Pullman, WA
USA
Dr Susmita Bose began her academic career in India, achieving her BSc and MSc in Chemistry at the University of Kalyani and Indian Institute of Technology (IIT) Kanpur, respectively. She then moved to the USA, where she was awarded her PhD in Physical-Organic Chemistry from Rutgers University in 1998. Since then, she has held various roles at Washington State University, including her current position as a Full Professor at the School of Mechanical and Materials Engineering. Here, she uses a combination of chemistry, engineering and biology to engineer materials for use in bone implants and drug delivery. Dr Bose’s research has made incredible contributions to the world of clinical material science, and she has achieved many awards and honours, including from the Royal Society of Chemistry, the National Academy of Inventors, and the prestigious Presidential Early Career Award for Scientist and Engineers (NSF-PECASE), given at the White House by the US President, for her interdisciplinary research on 3D-printed bone grafts and drug delivery. Dr Bose has published over 250 journal articles, 24 book chapters, 9 edited books, and 13 issued patents. Since 2011, her group’s research on 3D-printed ceramic bone scaffolds has been featured by the AP, BBC, NPR, CBS News, MSNBC, ABC News, and many other news outlets all over the world. Dr Bose is also passionate about training the next generation of scientists. In addition to teaching countless undergraduates, she has supervised over 45 PhD and MS students. Her advice to students is: ‘Dream big! Stay focused, plan, and work hard to achieve your dream. Use every opportunity you get that is aligned with your dream. Keep up with a hobby, stay healthy and celebrate life.’
CONTACT
E: sbose@wsu.edu
W: https://mme.wsu.edu/susmita-bose/
FURTHER READING
S Bose, D Banerjee, AA Vu, Ginger and Garlic Extracts Enhance Osteogenesis in 3D Printed Calcium Phosphate Bone Scaffolds with Bimodal Pore Distribution, ACS Applied Materials & Interfaces, 2022, 14, 12964.
A Bhattacharjee, S Bose, Zinc curcumin complex on fluoride doped hydroxyapatite with enhanced biological properties for dental and orthopedic applications, Journal of Materials Research, 2022, 37, 2009.
S Bose, D Ke, AA Vu, A Bandyopadhyay, SB Goodman, Thermal Oxide Layer Enhances Crystallinity and Mechanical Properties for Plasma-Sprayed Hydroxyapatite Biomedical Coatings, ACS Applied Materials & Interfaces, 2020, 12, 33465-33472.
S Bose, N Sakar, Natural Medicinal Compounds in Bone Tissue Engineering, Trends in Biology, 2020, 38, 404-417.
AA Vu, S Bose, Effects of vitamin D3 release from 3D printed calcium phosphate scaffolds on osteoblast and osteoclast cell proliferation for bone tissue engineering, RSC Advances, 2019, 9, 34847-34853.
S Tarafder, VK Balla, NM Davies, A Bandyopadhyay, S Bose, Microwave-sintered 3D printed tricalcium phosphate scaffolds for bone tissue engineering, Journal of Tissue Engineering and Regenerative Medicine, 2013, 7, 631-641.
S Bose, S Vahabzadeh, A Bandyopadhyay, 3-D printing of bone tissue engineering scaffolds, Materials Today, 2013, 16, 496-504.
S. Bose, S Tarafder, Calcium Phosphate Ceramic Systems in Growth Factor and Drug Delivery for Bone Tissue Engineering – A Review, Acta Biomaterialia, 2012, 8, 1401-1421.
S Bose, M Roy, A Bandyopadhyay, Recent advances in bone tissue engineering scaffolds, Trends in Biotechnology, 2012, 30, 546-554.

REPUBLISH OUR ARTICLES
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence (CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
SUBSCRIBE NOW
Follow Us
MORE ARTICLES YOU MAY LIKE
Dr Paul Robertson | Artificial Intelligence in the Cockpit: New Systems Could Help Prevent Aviation Accidents
Despite significant advances in aviation safety over recent decades, accidents still occur that could potentially be prevented with better warning systems. Dr Paul Robertson of Dynamic Object Language Labs, Inc. (DOLL) is leading groundbreaking research into how artificial intelligence could help pilots avoid dangerous situations. His team’s work reveals promising developments and important cautions about implementing AI in aircraft cockpits, with implications for the future of aviation safety.
Dr Silvia Remeseiro | Mapping the Epigenetic Landscape of Glioblastoma Progression
Glioblastoma, the most aggressive form of brain cancer, continues to challenge medical professionals with its poor survival rates. Recent groundbreaking research by Dr Silvia Remeseiro and her colleagues at Umeå University in Sweden has shed light on the complex epigenetic and chromatin-related mechanisms underlying the communication between neurons and glioma cells. This research opens new avenues for understanding and potentially treating this formidable disease.
Dr Markus Stumm | Advances in Screening for Genetic Abnormalities with Non-invasive Prenatal Testing
Non-invasive prenatal testing (NIPT) is a method of screening for genetic abnormalities in the unborn child through a simple blood sample taken from the mother. The non-invasive nature of the test has minimal to no risk to the mother and foetus and, since 2012, has been applied extensively around the world. As NIPT technology advances, Dr Markus Stumm of Medicover Genetics in Germany and his colleagues from Cyprus discuss the different techniques used, their strengths, their limitations and important considerations for pregnancy management.
New Directions for Reproductive Lifespan and Healthspan
Balancing starting a family with career goals is a difficult challenge many women have to face, which can lead to inequalities in various aspects of their lives. Dr Zhongwei Huang and the team at NUS Bia-Echo Asia Centre for Reproductive Longevity and Equality (ACRLE) are pioneers in reproductive health research. They work to improve female reproductive longevity and equality, exploring novel approaches to tackle fertility and conception problems, and ways to maintain optimal healthspan later in life.