Professor Dr André Fringer | Mrs Sabrina Stängle – The Voluntary Stopping of Eating and Drinking: Dying with Dignity?
To die with dignity is a common wish but not one that is easily granted. Professor Dr André Fringer and Mrs Sabrina Stängle, both of the Zurich University of Applied Sciences, are investigating the voluntary stopping of eating and drinking (VSED) as a means to hasten death as an alternative to active euthanasia. Their work is driving forward our understanding of the medical and ethical ramifications of this practice.
A Critical but Poorly Understood Issue
Removing the ambiguity surrounding euthanasia and assisted suicide could increase the quality of care received by those involved. For many chronically ill people, the desire to die is met with an onslaught of social, legal, and ethical consequences that may beg the question: isn’t there an easier way?
For the strong-willed patient, voluntarily abstaining from food and can lead to death by dehydration in anything from days to weeks. The time taken for death to occur depends on a multitude of factors including the health, age, and mental strength of the person involved. Whether this occurs explicitly and as a spoken wish by the patient, or implicitly, as a result of poor health or otherwise, the voluntary stopping of eating and drinking (VSED) is a significant cause of death that has not been extensively recognised in the medical community.
Professor Dr André Fringer and Mrs Sabrina Stängle, both of the Zurich University of Applied Sciences, intend to change this. They have conducted research on VSED for the last several years and brought the debate on whether VSED should be treated as suicide or natural death to Switzerland.

Suicide or Natural Death?
The issue of VSED, also known as ‘death fasting’, requires professional clarification to achieve uniform support across medical settings. Professor Fringer and Mrs Stängle explain that suicide, described by the World Health Organisation as ‘the act of deliberately killing oneself,’ may not be applicable to VSED if the individual already has a life-threatening illness. In this case, VSED could be simply thought of as speeding up the inevitable.
However, if an otherwise healthy person decides to undergo this process, it can be more accurately labelled as suicide since premature death ensues. This clarification becomes important when seeking the support of families or medical teams witnessing the dying process. The third position considers patient autonomy. As such, it may be considered unlawful or coercive to force food ingestion upon an unwilling, mentally well patient.
The legality and associated consequences of choosing to die in this manner vary from country to country. In Switzerland, considered a ‘right to die’ society, subjects who choose VSED are generally viewed as having experienced a natural death. In Germany and Austria, however, opinions are more divided and discussion around the subject is more controversial. Globally, the phenomenon of VSED exists, though is often hidden due to a lack of open discussion or integration into healthcare systems. For families or medical teams asked to support this request, it comes down to personal choice and the level of perceived suffering at hand.
Ultimately, and despite the surface-level autonomy and independence required, those choosing the VSED path require a palliative care model towards the end of their life. The ensuing vulnerability and loss of functionality that is experienced must be a key factor to be considered by interested parties. Professor Fringer and Mrs Stängle explain that the starting point of the individual’s health is what determines whether VSED leads to a natural or radical death.

Oral Nutrition Refusal Sub-types
Due to insufficient material existing on the VSED, Professor Fringer and Mrs Stängle aimed to identify and distinguish between different forms of oral nutrition refusal and different forms of VSED. Following media attention gathered during their interactions with healthcare professionals, the researchers received requests from people who had supported relatives through the VSED who wanted to share their experiences. Open-ended, semi-structured interviews were then conducted with these family members, who were asked to describe the full course of the VSED, including reasons for implementation and the decision-making process involved. Any complications which arose were also explored.
This process revealed that there is much more to the VSED than a simple decision to refrain from eating or drinking. The authors identified that nutrition refusal in VSED should be identified as separate from mental illness, eating disorders, natural death and hunger strike. VSED was also found to exist in implicit forms, driven by the various motives the individual wishing to die may have for refraining from fluids in secret and undetected by others. Thus, although VSED can often be a very explicit form of death involving spoken intent, the research by Professor Fringer and Mrs Stängle demonstrates that much more difficult to detect forms of food and liquid refusal also require better understanding.
During implicit VSED, the healthcare workers involved may misjudge the process and view it as a natural death. In this example, individuals often feel socially or emotionally isolated and may choose to refrain from food and liquids without explicitly expressing this decision. These patients either do not want to or cannot communicate their decision. This decision can be thought of in the context of ‘life fatigue’ as opposed to the desire for autonomy. The researchers saw this commonly in old age.
Overall, the researchers clearly showed that VSED is a multifaceted condition that must be distinguished from other forms of nutrition refusal. In particular, implicit and concealed VSED should become known as a form of nutrition refusal in order to avoid confusion with the natural dying process. Different forms of nutrition refusal close to VSED are associated with different needs, and professional support must be adapted accordingly.

A Palliative Care View
Professor Fringer and Mrs Stängle’s next step was to ascertain a comprehensive representative picture of VSED in Switzerland, on which no prior empirical data existed. Professor Fringer and Mrs Stängle created and distributed a trilingual survey (in German, French, and Italian) to Swiss healthcare personnel, the results of which would provide important information both about the occurrence of VSED, and also about its professional handling. The aim of this work was to help improve the quality of care received by patients opting for VSED, and to improve competence and confidence in associated healthcare staff.
Additionally, the team’s questionnaire aimed to gather details of healthcare workers’ attitudes towards VSED, including their willingness to participate in the practice. The survey was distributed to a variety of healthcare professionals, from GPs to nurses to paramedics, since interdisciplinary cooperation is essential for potential future standardisation of care.
Data analysis revealed that the VSED in these settings is mainly carried out by cancer patients (40.5%) or by people without any serious disease (28.9%). The underlying causes include fatigue (61%) and the fear of being dependent on others (59.5%). Death from the VSED was viewed as dignified by 57.5% of all professionals surveyed.
Looking to Nursing Homes
The team also created a cross-sectional study directed at heads of Swiss nursing homes to gather their experiences and opinions on VSED. Their online survey was answered by 34% of all nursing home heads, and data analysis revealed 1.7% of all patients in these settings died following VSED. Almost 70% of participants considered this phenomenon highly relevant in their daily work. Participants described the VSED as being more expected by older patients, and they tended to view it as a natural death which was accompanied by health professionals. As many as 92% of participants believed that patients undergoing VSED deserved the right to care, and overall, views toward the subject were positive.
In general, the survey found that healthcare professionals view VSED as a phenomenon of old age, rather than a formalised end-of-life practice. Professor Fringer and Mrs Stängle’s insight indicated the need for additional staff training and clearer positioning on this issue, which would provide essential clarity and better standardisation of care.

Family-centred Care
Alongside creating professional acceptance and integration of the VSED, Professor Fringer and Mrs Stängle explained the need for a family-centred care model to be established to help all those involved. Patients who choose the VSED will at some point depend on familial support, as well as nursing or medical aid. Whether individuals opt for the accompaniment of their relatives during their VSED process, or for the family to assist only with medical or legal formalities, some interaction is necessary between the patient, their family, and medical staff. To this end, Professor Fringer and Mrs Stängle developed a family-centred care model, which would take all of this into account and could improve the wellbeing of all involved in this process.
Professional Stance of Physicians
In recently published research, Professor Fringer and Mrs Stängle aimed to determine how often patients undergoing the VSED do so with the support and/or knowledge of their Swiss family physicians. In addition to this, they were interested in physicians’ attitudes and professional stances towards this issue.
After analysing results from 751 practising family physicians, the researchers determined that VSED was a well-known phenomenon among 81.9% of those investigated, with over one-third having accompanied at least one patient during VSED. Despite this, there is still a lack of in-depth knowledge on the subject required to appropriately advise patients and families concerned. In 2017, VSED accounted for 1.1% of all deaths that occurred in Swiss nursing homes or privately. The physicians classified this as a natural dying process (59.3%), passive euthanasia (32.0%), or suicide (5.3%).
Another recent paper by Professor Fringer and Mrs Stängle explored the experiences, personal attitudes, and professional stances of 1,681 Swiss health care professionals (including nursing directors, institute directors and head nurses) toward VSED using a standardised questionnaire. Findings indicated predominantly positive personal attitudes of professionals when confronted with VSED and desire to support the autonomy and self-determination of patients despite potentially holding moral reservations.
It is clear that further training and the development of basic practice recommendations relating to VSED is required to better support both healthcare personnel and patients. The awareness raised by Professor Fringer and Mrs Stängle is critical in paving the way for improved end-of-life care in Switzerland and across the globe.
Reference
https://doi.org/10.33548/SCIENTIA575
Meet the researchers

Professor Dr André Fringer, MScN, RN
ZHAW Zurich University of Applied Sciences
School of Health Professionals, Institute of Nursing
Winterthur
Switzerland
Professor Dr André Fringer completed his postdoctoral degree in 2011 in the Faculty of Health, Department of Nursing Science, at the Witten/Herdecke University in Witten, Germany. At the Institute of Nursing at the FHS St.Gallen, University of Applied Sciences in St.Gallen, Switzerland, he went on to serve as scientific head of degree for the Master of Advanced Studies in Palliative Care programme, as well as both project manager and deputy director in the Institute of Applied Nursing-Science. Today, he is a Family-Centred Care Professor, alongside co-heading his university’s Nursing Science Research Unit, and heading the MSc in Nursing course at the Institute of Nursing at the Zurich University of Applied Sciences in Winterthur, Switzerland. Professor Fringer is now working with collaborators to investigate end of life nutrition and the onset of familial caregiving.
CONTACT
E: andre.fringer@zhaw.ch
W: zhaw.ch/en/about-us/person/frin/

Mrs Sabrina Stängle, MSc, RN
ZHAW Zurich University of Applied Sciences
School of Health Professionals, Institute of Nursing
Winterthur
Switzerland
Mrs Sabrina Stängle is a Research Associate at the Zurich University of Applied Sciences (ZHAW) and PhD-student at Witten/Herdecke University in Witten, Germany. Since completing her MSc in Health and Nursing Sciences in 2016 at Martin Luther University Halle-Wittenberg, Germany, she has been undertaking a PhD in Nursing Sciences which enabled her to join ZHAW in 2018. She has contributed to a number of research projects and peer-reviewed publications involving end-of-life nutrition and palliative care, and has extensive experience lecturing in nursing and its related fields. Her research interests lie in palliative care, loneliness, and end-of-life decisions.
CONTACT
E: sabrina.staengle@zhaw.ch
W: zhaw.ch/en/about-us/person/fehs/
KEY COLLABORATORS
Professor Dr Wilfried Schnepp, Head of Department for Family-Oriented and Community Care, Witten/Herdecke University (deceased 14th February 2020)
Dr Daniel Büche MD, Chief physician at Cantonal Hospital St.Gallen
Dr Christian Häuptle, Head of Family Medicine at Cantonal Hospital St. Gallen (retired)
Jasmin Meichlinger, Research Associate at FHS St. Gallen University of Applied Sciences
SPONSORS:

COLLABORATORS:

RESEARCHERS’ INSTITUTION: 
Want to republish our articles?
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence
(CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
More articles you may like
Dr Lifei Wang | Can Species Distribution Models Inform Us About Future Ecosystems?
The world is buzzing with news about how human activities and climate shifts are reshaping our ecosystems. Have you ever wondered how life will adapt to this rapidly changing world? Ecologists might be able to predict how different species will live in future using computer simulations. Dr Lifei Wang at the University of Toronto Scarborough investigates how different stimulations work under varying conditions to provide new insights into what may lie ahead.
Dr Yong Teng | Improving the Outlook for Head and Neck Cancer Patients
Dr Yong Teng at the Emory University School of Medicine is working with colleagues to overcome the high mortality of individuals diagnosed with cancers affecting the head and neck. One of his approaches is based on understanding the particular mechanisms of the ATAD3A gene, which new insights suggest are closely related to cancers affecting the head and neck.
Dr Tsun-Kong Sham – Dr Jiatang Chen – Dr Zou Finfrock – Dr Zhiqiang Wang | X-Rays Shine Light on Fuel Cell Catalysts
Understanding the electronic behaviour of fuel cell catalysts can be difficult using standard experimental techniques, although this knowledge is critical to their fine-tuning and optimisation. Dr Jiatang Chen at the University of Western Ontario works with colleagues to use the cutting-edge valence-to-core X-ray emission spectroscopy method to determine the precise electronic effects of altering the amounts of platinum and nickel in platinum-nickel catalysts used in fuel cells. Their research demonstrates the potential application of this technique to analysing battery materials, catalysts, and even cancer drug molecules.
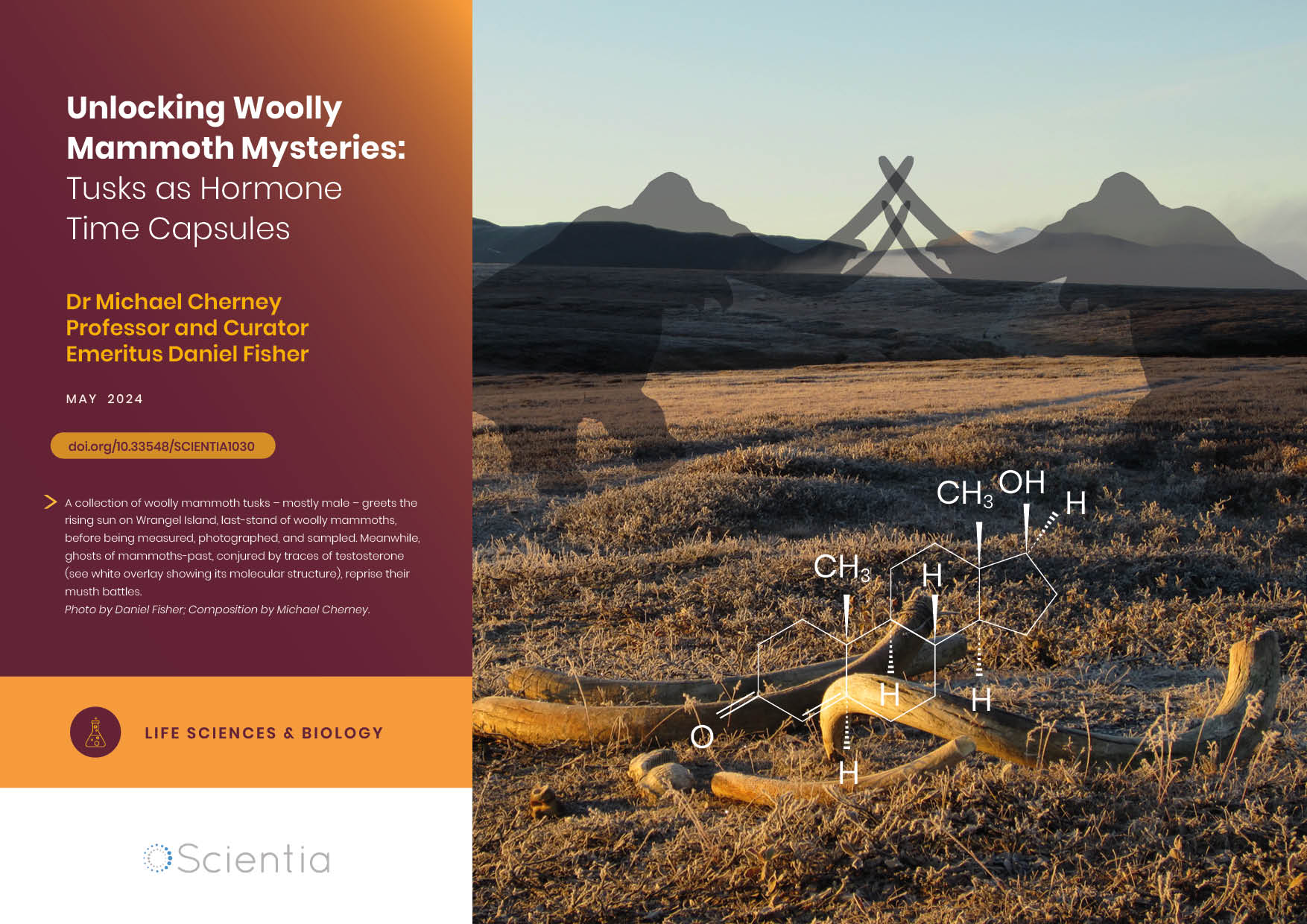
Dr Michael Cherney – Professor Daniel Fisher | Unlocking Woolly Mammoth Mysteries: Tusks as Hormone Time Capsules
The impressive tusks found on proboscideans (the order of mammals that includes elephants, woolly mammoths, and mastodons) are like time capsules, preserving detailed records of their bearers’ lives in the form of growth layers and chemical traces. Frozen in time for thousands of years, these layers can unlock secrets about the lives of long-extinct relatives of modern elephants. Dr Michael Cherney and Professor Daniel Fisher from the University of Michigan used innovative techniques to extract and analyse steroid hormones preserved in woolly mammoth tusks. This ground-breaking work opens new avenues for exploring the biology and behaviour of extinct species.