Professor Michael Bukrinsky | Human Immunodeficiency Virus Co-morbidities: How Lipid Homeostasis Alterations Lead to Cardiovascular and Neurological Disorders
Although human immunodeficiency virus (HIV) is still prevalent worldwide, life-saving antiretroviral drugs can now prevent an infection from progressing into acquired immunodeficiency syndrome (AIDS). Nevertheless, people who are HIV-positive are still at increased risk of developing neurological disorders and cardiovascular diseases, known as co-morbidities. Professor Michael Bukrinsky from the George Washington University in Washington DC works to understand the underlying biological mechanisms that lead to these disorders. His research has produced interesting results that demonstrate the role of altered lipid (cholesterol) homeostasis in HIV-infected cells and how this comes to pass.
Uncovering Causes and Proposing Solutions
Over 37 million people worldwide are infected with human immunodeficiency virus (HIV), and an estimated 1.7 million of these are children. The virus replicates by entering immune cells, particularly CD4+ T cells and macrophages, and multiplying inside them. Once new HIV virions have been produced, they burst out of the host cell to repeat replication, which kills the cell in the process. Due to viral reproduction in the immune cells, the immune systems of people infected with HIV are greatly impacted and they become susceptible to additional diseases.
HIV is spread via certain bodily fluids and can, therefore, be transmitted during unprotected sex, sharing needles and during pregnancy or breastfeeding. Although initial infection may result in a few weeks of flu-like symptoms, many people usually will not present any symptoms for a number of years. However, if it is left untreated, HIV leads to acquired immunodeficiency syndrome (AIDS), whereby the immune system is so damaged and unable to repair itself, that previously minor infections and illnesses become life-threatening.
Thankfully, treatments have been found that allow those living with HIV infection to live long, healthy lives. These treatments come in the form of antiretroviral drugs, which prevent the virus from infecting new T cells and macrophages and in turn, allow the immune system to repair itself. Eventually, taking these tablets every day results in an undetectable viral load, meaning that the amount of HIV in the body is so low that it cannot be detected by a test and the risk of transmission is minimal.
Although impressive progress has been made to improve the lives of those living with HIV/AIDS, research has shown that they still have a high risk of co-morbidities. These are ailments that are not caused by a damaged immune system, but by other, HIV-associated, yet less clear mechanisms. For example, people who are HIV-positive are more likely to have high blood pressure and high cholesterol, develop heart disease, kidney disease, neurological issues and cancer.
Uncovering the reasons behind and solutions to these troubling HIV co-morbidities is Professor Michael Bukrinsky from the Department of Microbiology, Immunology and Tropical Medicine at the George Washington University in Washington DC. In collaboration with scientists across the globe, Professor Bukrinsky is working to elucidate the molecular mechanisms behind these comorbidities so that they can be targeted with therapies.

Lipid Homeostasis in HIV-infected Macrophages
The role of cholesterol in cardiovascular diseases has been well established. However, prior to Dr Bukrinsky’s studies, there has been little investigation into the impact HIV has on cholesterol homeostasis. Cholesterol is an essential lipid (or fat) in the body that aids in the synthesis of cell membranes, hormones and vitamins. But when there is an imbalance between the high-density lipoprotein (often called ‘good’ HDL) and low-density lipoprotein (‘bad’ LDL) forms, the risk of cardiovascular diseases increases. An excess of LDL in the bloodstream also frequently leads to atherosclerosis, which is a thick deposit of cholesterol, fat and calcium within an artery. As this deposit (known as a plaque) grows, the artery narrows and a blood clot trapped in the small space can result in a heart attack or stroke.
Professor Bukrinsky and his colleagues carried out research to discover why this is so common in HIV patients. His team included Professor Dmitri Sviridov at the Baker Heart and Diabetes Institute, Dr Zahedi Mujawar (Astra Zeneca, a former graduate student), and Professor Michael Fitzgerald at Harvard Medical School. They discovered that the virus inhibits a cholesterol transporter protein in macrophages – a type of white blood cell in the immune system. This transporter is called ATP-binding cassette transporter A1 (ABCA1) and when it is prevented from functioning normally, cholesterol cannot leave the macrophage cell. The inhibition of cholesterol efflux is a condition previously documented as causing high atherosclerosis risk.
The team ascertained that in HIV-infected cells, this inhibition event was regulated by an HIV protein called Nef, and further investigation found that two biological mechanisms were responsible. First, Nef binds to and down-regulates ABCA1, meaning that it reduces its abundance – and thus, its ability to facilitate cholesterol efflux. Second, Nef interacts with another cellular protein, calnexin, which regulates glycosylation and maturation of ABCA1. As a result, ABCA1 cannot mature and is sent to the degradation pathway as a cellular defence reaction to the accumulation of immature proteins. Together, these mechanisms cause the reduction of ABCA1 and prevent the transfer of cholesterol to apolipoprotein A-I, a major component of HDL cholesterol. These processes result in an imbalance of blood lipoprotein cholesterol.
Studies by Dr Brichacek in Professor Bukrinsky’s group further demonstrated that the described above effects of Nef are also reproduced by treating cells with Nef-containing extracellular vesicles (EVs). These vesicles are produced by HIV-infected cells and persist in infected individuals even when the virus is undetectable. The reason for this is that the antiretroviral drugs used to treat infected patients prevent new infections, but do not block low-level production of Nef in infected cells. Circulation of these Nef-containing EVs may be the reason for the persistence of co-morbidities in successfully treated patients with undetectable HIV load.
Professor Bukrinsky’s studies also showed that HIV-infected and Nef-EV-treated macrophages accumulated a significant amount of lipids within them. This gave them a resemblance to foam cells, a type of macrophage that sticks to blood vessel walls, internalising LDL and facilitating atherosclerosis formation. In addition, cholesterol enrichment leads to changes in the cellular membrane, increasing the size and number of cholesterol-rich islets called ‘lipid rafts’. These lipid rafts are places where cellular receptors sensing and responding to inflammation accumulate, making cholesterol-rich macrophages overresponsive to inflammatory stimuli. This mechanism may underlie another important cause of atherosclerosis in HIV-infected individuals, persistent inflammation. When Professor Bukrinsky stimulated cholesterol efflux from HIV-infected macrophages, the HIV viruses that were produced inside were much less infectious. This shows that the virus requires a certain, high cholesterol level within its host cell to maximise its replication ability, and HIV achieves this by preventing cholesterol efflux.
These exciting results revealed brand-new mechanisms by which HIV Nef regulates intracellular lipid homeostasis within HIV-infected cells and cells encountering Nef-containing EVs. In this way, Professor Bukrinsky’s work showed how HIV infection of macrophages contributes to the co-morbidity of atherosclerosis and its associated risks. A subsequent study with Dr Ruth Hunegnaw (National Institutes of Health, a former graduate student) and Professor Alexei Adzhubei (Engelhardt Institute of Molecular Biology) and Amol Kulkarni (Howard University) revealed that specific interactions with Nef could be blocked and therefore potentially targeted with drugs to prevent HIV from impacting cholesterol homeostasis and thus, reduce the risk of atherosclerosis.

Neurodegeneration in HIV
Professor Bukrinsky’s group has further studied lipid rafts, the solid structures in the plasma membrane and the barrier between a cell and its surroundings. These rafts are full of cholesterol molecules and help to mediate interactions with the cell’s environment. Whilst these interactions are usually beneficial, pathogens can take advantage of lipid rafts and use and even modify them to facilitate their own replication. Lipid raft therapy can be implemented as a treatment for viral infections by reducing unwanted modifications of lipid rafts or preventing viral interactions with these regions, and Professor Bukrinsky suggests this may even be an effective treatment for COVID-19.
Similar to atherosclerosis, lipid raft structures are key players in HIV-associated neurocognitive disorders (HAND), which are very frequent even in HIV patients receiving treatment. HAND is often seen as behavioural changes, declining cognitive function and motor impairment, and Professor Bukrinsky studied the role of Nef in HAND.
His studies showed that the Nef protein secreted from HIV-infected cells in EVs was rapidly internalised by neural and glial cells, and as seen in previous experiments, reduced ABCA1 abundance and cholesterol efflux, and also increased the number of modified lipid rafts in the plasma membrane.
Nef EVs also caused the increase and redistribution of amyloid precursor protein (APP) and Tau to lipid rafts, both of which are associated with brain disorders. With the addition of the activation of inflammatory pathways, Professor Bukrinsky observed consequent neuronal functional impairment which was reversed when the lipid rafts were disrupted. These findings were supported by evidence from brain tissue of deceased HIV patients with HAND, which showed lower levels of ABCA1 and more lipid rafts compared to HIV-negative brain tissue. Additionally, an abundance of Nef in the HIV-positive tissue correlated with APP and Tau levels. Finally, Jessica Schenck, a graduate student in Bukrinsky’s laboratory, demonstrated that Nef-carrying EVs cause demyelination of the brain. Myelin forms cholesterol-rich sheaths of neurons required for neuronal functions, and cholesterol transport is essential for their maintenance.
As a result, Professor Bukrinsky concluded that the cholesterol homeostasis alterations arising from the presence of Nef in the brains of HIV-infected people may contribute to neurodegeneration and HAND. Understanding the underlying mechanisms of disease facilitates the development of therapies to target them, and Professor Bukrinsky’s research suggests that treatments preventing Nef-induced alterations of cholesterol homeostasis and/or normalising lipid raft structure may reverse HAND.
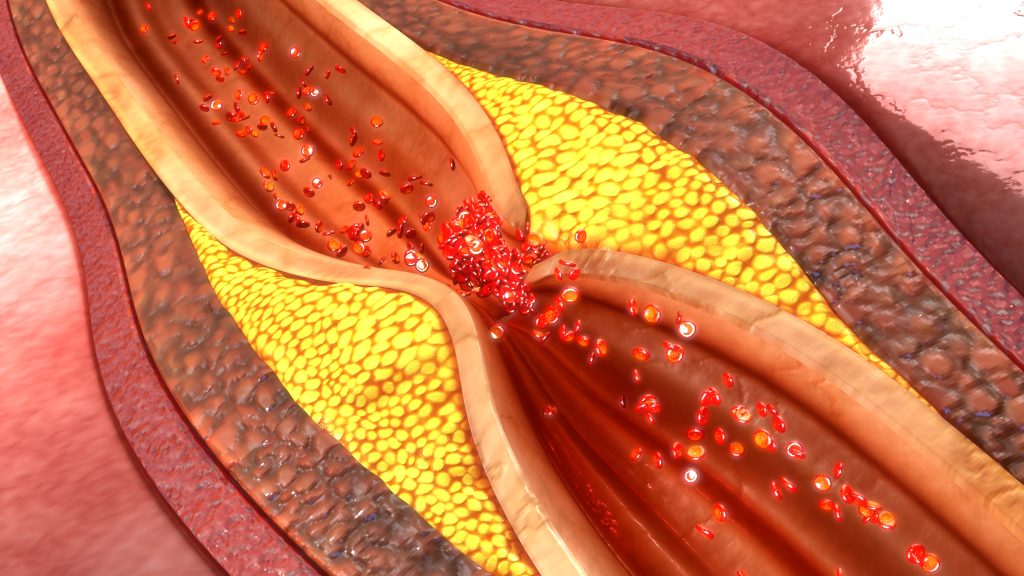
Illustration of coronary artery plaque
Discovering HIV-Specific Memory
The most recent discovery by Larisa Dubrovsky, a scientist in Professor Bukrinsky’s group demonstrated that cells treated with Nef EVs acquire a memory of this encounter. This memory is maintained by epigenetic (not involving genetic material) changes that regulate the expression of pro-inflammatory and lipid metabolism genes. As a result, cells, and in particular macrophages, become overresponsive to inflammatory stimuli.
This mechanism supplements and potentiates the mechanisms described above. The length of this memory is extended by the possibility that Nef EVs affect progenitor cells in the bone marrow, thus potentially impacting cells produced from these progenitors for a very long time. This finding adds another complication to be considered in the efforts to cure HIV infection. Indeed, besides silencing HIV, either by eliminating it from the body or by permanently blocking the virus from producing proteins and nucleic acids, care should be taken to clear the memory formed during the encounter with the virus or Nef EVs. Professor Bukrinsky’s studies support the development of approaches aimed at reversing or blocking the establishment of this memory.
Discovering and Blocking a Pro-inflammatory Protein
While Professor Bukrinsky has devoted much of his research to HIV and its co-morbidities, his laboratory explores other avenues of research as well. These include obtaining a better understanding of inflammatory diseases, the biological interactions that cause them and how they can also be targeted by drugs. Studies with Professors Yurchenko (University of Ostrava) and Sherry (Feinstein Institutes) identified that extracellular proteins called cyclophilins and their receptor on immune cells called CD147 regulate various inflammatory disorders such as acute lung inflammation, cardiovascular disease and rheumatoid arthritis. CD147- mediated signalling by cyclophilins guide immune cells to the sites of inflammation.
Therefore, Professor Bukrinsky and his colleagues believed that targeting these interactions would be a promising possibility for anti-inflammatory therapeutics. Together with Professors Stephanie Constant (National Institutes of Health) and Gunter Fischer (Max Planck Research Unit) he developed and patented an exciting new drug that blocks the action of extracellular cyclophilin A. They hope that this could be used to alleviate the symptoms of both acute and chronic inflammation and mitigate the subsequent risks associated with it.
SHARE
DOWNLOAD E-BOOK
WATCH THE ANIMATION
LISTEN TO THE AUDIO
REFERENCE
https://doi.org/10.33548/SCIENTIA836
MEET THE RESEARCHER

Professor Michael I. Bukrinsky
Department of Microbiology, Immunology and Tropical Medicine
George Washington University School of Medicine and Health Sciences
Washington DC
USA
Professor Michael Bukrinsky received his first degree in Biochemistry from the Second Moscow State Medical Institute before completing a PhD at the Institute of Molecular Biology in the USSR Academy of Sciences. Professor Bukrinsky has served in many teaching and research roles throughout his career and currently works at the George Washington University School of Medicine and Health Sciences in Washington DC. Here, he is a Professor in the Department of Microbiology, Immunology & Tropical Medicine and also Professor in Biochemistry and Molecular Medicine. His studies investigate successfully treated HIV cases that still result in persistent co-morbidities, and have been widely recognised with prestigious awards.
CONTACT
W: https://mme.wsu.edu/jinwen-zhang/
KEY COLLABORATORS
Dmitri Sviridov (Baker Heart and Diabetes Research Institute, Australia)
Ilya Leventhal (University of Virginia, USA)
William Tyor (Emory University, USA)
Michael Fitzgerald (Harvard Medical School, USA)
Yury Miller (University of California San Diego, USA)
Alexei Adzhubei (Engelhardt Institute of Molecular Biology, Russia)
FUNDING
National Institutes of Health
FURTHER READING
T Pushkarsky, A Ward, A Ivanov, et al., Abundance of Nef and p‑Tau217 in Brains of Individuals Diagnosed with HIV‑Associated Neurocognitive Disorders Correlate with Disease Severance, Molecular Neurobiology, 2021. DOI: https://doi.org/10.1007/s12035-021-02608-2
MI Bukrinsky, N Mukhamedova, D Sviridov, Lipid rafts and pathogens: the art of deception and exploitation, Journal of Lipid Research, 2020, 61(5), 601–610. DOI: https://doi.org/10.1194/jlr.TR119000391
M Ditiatkovski, N Mukhamedova, D Dragoljevic, et al., Modification of lipid rafts by extracellular vesicles carrying HIV-1 protein Nef induces redistribution of amyloid precursor protein and Tau, causing neuronal dysfunction, Journal of Biological Chemistry, 2020, 295(38), 13377–13392. DOI: https://doi.org/10.1074/jbc.RA120.014642
D Sviridov, YI Miller, RA Ballout, et al., Targeting lipid rafts – a potential therapy for COVID-19, Frontiers in Immunology, 2020, 11. DOI: https://doi.org/10.3389/fimmu.2020.574508
R Hunegnaw, M Vassylyeva, L Dubrovsky, et al., Interaction between HIV-1 Nef and calnexin: from modeling to small molecule inhibitors reversing HIV-induced lipid accumulation, Arteriosclerosis, Thrombosis and Vascular Biology, 2016, 36(9), 1758–1771. DOI: https://doi.org/10.1161/ATVBAHA.116.307997
M Bukrinsky, Extracellular cyclophilins in health and disease, Biochimica et Biophysica Acta (BBA)-General, 2015, 1850(10), 2087-2095. DOI: https://doi.org/10.1016/j.bbagen.2014.11.013
V Yurchenko, S Constant, E Eisenmesser, M Bukrinsky, Cyclophilin–CD147 interactions: a new target for anti-inflammatory therapeutics, Clinical & Experimental Immunology, 2010, 160(3), 305–317. DOI: https://doi.org/10.1111/j.1365-2249.2010.04115.x
Z Mujawar, H Rose, MP Morrow, et al., Human Immunodeficiency Virus Impairs Reverse Cholesterol Transport from Macrophages, PLoS Biology, 2006, 4(11), e365. DOI: https://doi.org/10.1371/journal.pbio.0040365

REPUBLISH OUR ARTICLES
We encourage all formats of sharing and republishing of our articles. Whether you want to host on your website, publication or blog, we welcome this. Find out more
Creative Commons Licence (CC BY 4.0)
This work is licensed under a Creative Commons Attribution 4.0 International License. 
What does this mean?
Share: You can copy and redistribute the material in any medium or format
Adapt: You can change, and build upon the material for any purpose, even commercially.
Credit: You must give appropriate credit, provide a link to the license, and indicate if changes were made.
SUBSCRIBE NOW
Follow Us
MORE ARTICLES YOU MAY LIKE
International Isocyanate Institute | TDI-induced Asthma: Reanalysing Data to Find Hidden Trends
Even if you’ve never heard of them, you’ve used polyurethanes. Producing them requires toluene diisocyanates, which may/can induce asthma when inhaled. A 5-year study claimed to conclude that cumulative TDI exposure over time was indicative of asthma incidence. However, a reanalysis by a team at the International Isocyanate Institute points the finger instead at the frequency of unprotected high-exposure events, like accidental spills or plant maintenance. This finding guides the way for future advances in worker safety.
Training Deep Learning AI to Predict microRNA-Gene Interactions
Non-coding microRNAs (miRNAs) have important regulatory functions but are also implicated in various diseases. Mr Seung-won Yoon, PhD candidate at Chungnam National University, Republic of Korea, is training deep learning AI models to predict miRNA-gene associations. His research has implications for understanding disease pathogenesis, particularly cancer, and repurposing drugs for untreatable diseases.
Improving the Immune Response with Intraoperative Cell Salvage
Undergoing surgery comes with many risks. Numerous factors can influence the outcome, from the choice of anaesthesia to the type of operation. Long and complex procedures can require blood transfusions, which introduce yet another risk factor to the mix. Dr Michelle Roets from the Royal Brisbane and Women’s Hospital in Queensland seeks to help mitigate these risks through intraoperative cell salvage, a different type of blood transfusion which could revolutionise surgical outcomes.
Dr Wilber Sabiiti | Battling Tuberculosis whilst Maintaining the Respiratory Microbiome
In the world of respiratory health, treating tuberculosis infections is an ongoing challenge. Dr Wilber Sabiiti from the University of St Andrews in the UK, delves into the impact of various tuberculosis treatments on the intricate community of microorganisms residing in the respiratory tract. He explores the impact of seven different treatment regimens and their effects on the microbiome, which is crucial for maintaining respiratory health and well-being.